Acetaminophen and Liver Disease: Safe Dosing to Avoid Hepatotoxicity
 Jan, 23 2026
Jan, 23 2026
Acetaminophen Safety Calculator
This calculator helps determine your safe daily acetaminophen limit based on your liver health and alcohol consumption. Remember: hidden sources (cold medicines, sleep aids) make up the majority of acetaminophen overdoses.
Your current intake is within safe limits.
Acetaminophen is in almost every medicine cabinet. You know it as Tylenol, but it’s also hidden in cold meds, pain relievers, and even sleep aids. It’s cheap, effective, and widely available. But if you have liver disease-or even just drink alcohol occasionally-taking it the "normal" way could be dangerous. You don’t need to overdose on purpose to hurt your liver. Sometimes, just following the label isn’t enough.
Why Acetaminophen Is Risky for Liver Disease
Your liver breaks down acetaminophen into harmless byproducts. But when you take too much, or your liver is already damaged, that process goes wrong. A toxic compound called NAPQI builds up. Normally, your liver uses glutathione to neutralize it. But if you’ve got liver disease, your glutathione levels are low. That means NAPQI starts eating away at liver cells. One study found that people with chronic liver disease can develop serious damage even at doses under 3,000 mg per day. That’s less than six extra-strength Tylenol pills.The Numbers That Matter
The standard daily limit for healthy adults is 4,000 mg. But that’s not safe for everyone. For people with liver disease, the real limit is closer to 2,000-3,000 mg. And if you drink alcohol regularly-even just a few drinks a week-that number drops even lower. Alcohol slows down how your liver processes acetaminophen and depletes glutathione faster. The combination can turn a normal dose into a toxic one.Here’s what the numbers look like:
- Healthy adult max: 4,000 mg/day (but not recommended for long-term use)
- Adult with liver disease: 2,000-3,000 mg/day
- With alcohol use: Under 2,000 mg/day
- Single toxic dose: Over 7.5-10 grams
- Children’s max: 80 mg/kg/day
And here’s the scary part: many people hit those toxic levels without realizing it. They take two Tylenol tablets (1,000 mg) for a headache. Then they take a cold medicine with acetaminophen for a stuffy nose. Then they take a sleep aid with it at night. Suddenly, they’ve taken 4,500 mg in one day. No one meant to overdose. But it happens every day.
Hidden Acetaminophen Is the Biggest Danger
You won’t always see "acetaminophen" on the label. Look for "APAP"-that’s the abbreviation. It’s in more than 600 medications. Vicodin, Percocet, Nyquil, Sudafed, Midol, Excedrin, and even some cough syrups. If you’re taking more than one product at a time, you’re probably doubling up without knowing it. A 2018 study found that acetaminophen is the top reason people call poison control centers in the U.S. That’s not because people are trying to hurt themselves. It’s because they didn’t know what they were taking.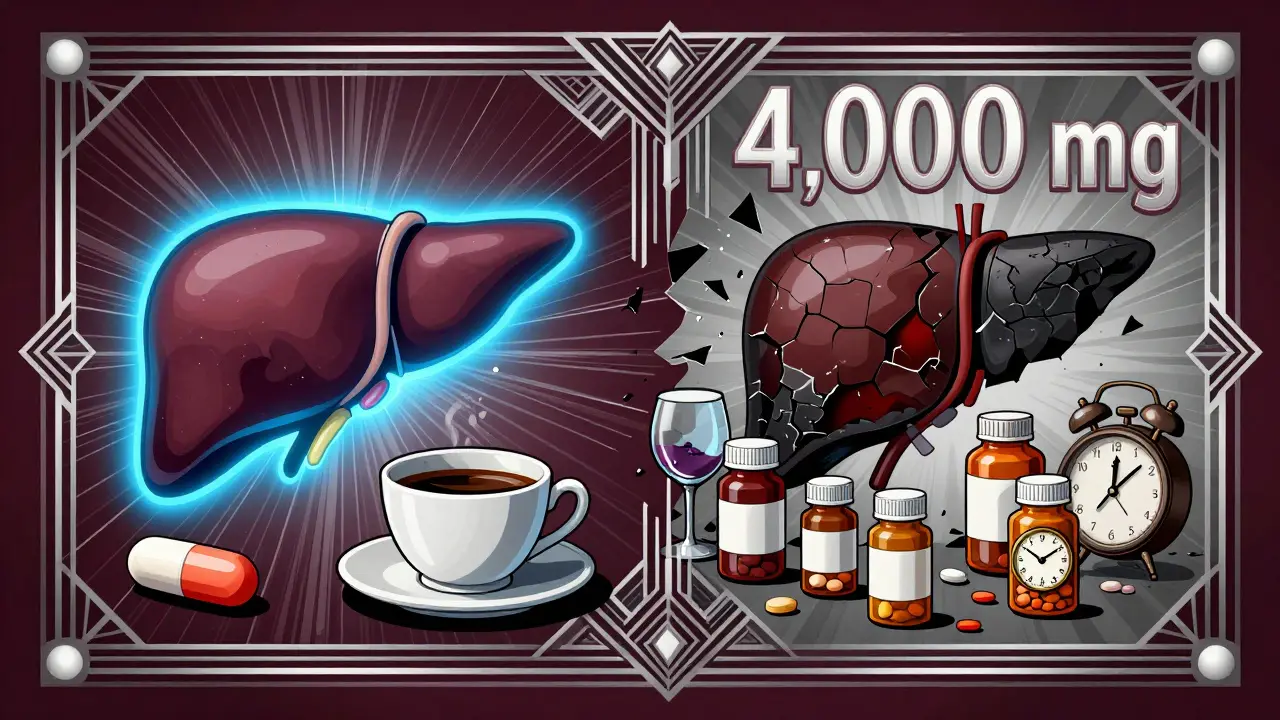
What If You Already Have Liver Disease?
If you have hepatitis, fatty liver, cirrhosis, or any chronic liver condition, you need to treat acetaminophen like a controlled substance. Talk to your doctor before taking it at all. Some patients with mild liver disease can still use it safely at reduced doses. Others can’t use it at all. There’s no one-size-fits-all answer. But here’s what’s clear: if your liver is already struggling, you don’t need extra stress.Don’t assume your doctor knows you’re taking it. Many patients don’t mention over-the-counter meds. But your doctor needs to know. Even if you think it’s "just Tylenol," it’s not harmless when your liver is compromised.
Alcohol and Acetaminophen: A Deadly Mix
Drinking alcohol while taking acetaminophen is like pouring gasoline on a small fire. It doesn’t matter if you drink on weekends or just one glass with dinner. Chronic alcohol use-even moderate-makes your liver more vulnerable. The risk isn’t just from binge drinking. It’s from daily use. One study showed that people who drank regularly and took 3,000 mg of acetaminophen daily had a much higher chance of liver damage than those who didn’t drink.There’s no safe amount of alcohol when you’re taking acetaminophen long-term. If you’re using it for pain, cut out alcohol. If you’re using it for a cold, skip the beer. The combination can cause sudden, severe liver injury-even if you’ve taken it safely for years.
What to Do If You Accidentally Overdose
If you think you’ve taken too much-whether it’s one big dose or several days of too much-you need help fast. Don’t wait for symptoms. Nausea, vomiting, and fatigue don’t show up until liver damage is already happening. The antidote, acetylcysteine (NAC), works best if given within 8 hours. It’s still helpful up to 16 hours after ingestion.Go to the ER. Tell them you took acetaminophen. They’ll check your blood level and use the Rumack-Matthew nomogram to decide if you need treatment. Don’t be embarrassed. This isn’t about drug abuse. It’s about confusion. Most overdose cases are unintentional.
How to Use Acetaminophen Safely
If you have liver disease-or even if you don’t but want to be careful-follow these steps:- Check every medicine label. Look for "acetaminophen" or "APAP."
- Add up the total from all sources. Don’t just count Tylenol.
- Never exceed 3,000 mg per day if you have liver disease.
- Avoid alcohol completely while taking it.
- Use a pill organizer or app to track doses. Don’t rely on memory.
- For children, use the syringe that comes with the liquid-not a kitchen spoon.
- Ask your pharmacist to review all your meds. They see what you might miss.
Alternatives to Acetaminophen
If you’re worried about liver damage, talk to your doctor about other pain relievers. NSAIDs like ibuprofen or naproxen are options-but they come with their own risks, like stomach bleeding or kidney strain. For chronic pain, physical therapy, heat packs, or even low-dose antidepressants may help. There’s no perfect substitute, but there are safer paths if you’re working with a provider who knows your history.Bottom Line: It’s Not About Being Careful. It’s About Being Informed.
Acetaminophen isn’t evil. It’s a useful drug. But it’s not safe for everyone. If you have liver disease, you’re not being overly cautious by avoiding it. You’re being smart. The 4,000 mg limit was set for healthy people. It doesn’t apply to you. Your liver is already working harder. Don’t ask it to do more.Read labels. Track doses. Talk to your doctor. Skip the alcohol. And if you’re ever unsure-don’t guess. Call your doctor or go to the ER. One mistake can change your life. But with the right information, you can avoid it entirely.
Can I take acetaminophen if I have fatty liver disease?
Yes, but with strict limits. Most doctors recommend no more than 2,000-3,000 mg per day. Avoid alcohol completely. Talk to your doctor before starting, because even low doses can cause harm if your liver is already inflamed or scarred. Some patients with advanced fatty liver disease may need to avoid it entirely.
Is Tylenol Extra Strength safer than regular Tylenol?
No. Tylenol Extra Strength contains 500 mg per pill, compared to 325 mg in regular. That means you reach the daily limit faster. In fact, the manufacturer recommends a maximum of 3,000 mg per day for Extra Strength-not 4,000 mg. Taking six pills a day (3,000 mg) is already the upper limit. Going beyond that increases your risk of liver damage, especially if you have liver disease or drink alcohol.
What happens if I take too much acetaminophen by accident?
You might not feel sick right away. Symptoms like nausea or fatigue can take 12-24 hours to appear. By then, liver damage may already be happening. The antidote, acetylcysteine, works best if given within 8 hours. Go to the ER immediately if you suspect an overdose-even if you feel fine. Don’t wait. Blood tests and the Rumack-Matthew nomogram will tell doctors if you need treatment.
Can children with liver disease take acetaminophen?
Children with liver disease should only take acetaminophen under a doctor’s supervision. The standard pediatric dose is 10-15 mg/kg per dose, but this may need to be lowered. Never use a kitchen spoon to measure liquid-always use the syringe provided. Overdose in children can lead to acute liver failure faster than in adults. If you’re unsure, ask your pediatrician for a safe dose chart.
Does taking acetaminophen for a few days hurt my liver?
For a healthy person, short-term use at recommended doses is usually safe. But if you have liver disease, even a few days of 3,000-4,000 mg can cause harm. Repeated supratherapeutic dosing-taking a little too much over several days-is a common cause of liver injury. It’s not just about one big overdose. It’s about cumulative exposure. If you’re taking it for more than a week, talk to your doctor.
Can I use acetaminophen while pregnant if I have liver disease?
Acetaminophen is still considered the safest pain reliever during pregnancy, even for women with mild liver disease. But the same rules apply: stay under 3,000 mg per day, avoid alcohol, and don’t combine it with other medications containing acetaminophen. Always consult your OB-GYN or hepatologist before taking it. IV acetylcysteine is safe during pregnancy if overdose occurs.
How do I know if my liver is damaged from acetaminophen?
Early signs are vague: nausea, loss of appetite, fatigue, and mild abdominal pain. Later signs include yellow skin (jaundice), dark urine, confusion, and swelling in the abdomen. But by then, damage is often severe. The only way to know for sure is a blood test. Liver enzymes (ALT, AST) rise sharply after overdose. If you’ve taken too much and feel off, get tested-even if you don’t think it’s serious.
Juan Reibelo
January 24, 2026 AT 12:12Man, I had no idea APAP was everywhere. I took Nyquil for a cold last week and then hit up Tylenol for my back pain. Thought I was being smart. Now I’m sweating bullets checking every bottle in my cabinet. Thanks for the wake-up call.
Karen Conlin
January 24, 2026 AT 19:49This is why we need better labeling laws. Not everyone reads tiny print. I’ve seen grandparents take three different meds with acetaminophen because the labels say ‘pain relief’ and they assume it’s different. We need big, bold, red text: ‘ACETAMINOPHEN - DO NOT MIX.’ And pharmacies should scan your meds and warn you before you check out. It’s not rocket science.
asa MNG
January 24, 2026 AT 20:50bro i just took 2 tylenol and a cold pill and now i’m scared 😭 i thought i was fine bc i’ve done it for years… why is this just now a thing?? 🤯 maybe the gov is hiding the truth??
Chloe Hadland
January 26, 2026 AT 01:40I’ve been on liver meds for years and I always just took one Tylenol if I needed it. Didn’t think twice. This post made me call my doctor today. She said I’m good with 2,000 mg max. Feels good to be informed.
Michael Camilleri
January 26, 2026 AT 10:55People are lazy. You don’t read labels. You don’t ask questions. You just pop pills like candy. Then you wonder why your liver is failing. This isn’t a conspiracy. It’s basic biology. If you can’t be responsible for your own body, don’t blame the medicine.
Darren Links
January 26, 2026 AT 20:11Who even decided 4,000 mg was safe? Probably some pharma exec in a suit who’s never had a liver. This whole thing is rigged. They want you dependent on their meds. Wake up. The system doesn’t care if you live or die.
Helen Leite
January 27, 2026 AT 09:53They put acetaminophen in everything because they want us to get liver damage. Then they sell us transplants. Big Pharma is running a death cult. I don’t take anything with APAP anymore. Not even one pill. 🚫💊
Marlon Mentolaroc
January 28, 2026 AT 20:16Interesting. I work in pharmacy and we see this all the time. The real issue? People think ‘OTC’ means ‘harmless.’ It doesn’t. Even water can kill you if you drink too much. Acetaminophen is just the most common unintentional poison. We give out pamphlets. No one reads them. Sad.
Gina Beard
January 30, 2026 AT 01:06Knowledge is power. But only if you use it.
Don Foster
January 31, 2026 AT 18:39You think you’re safe with 3000mg? That’s still dangerous if you’re not a genetic outlier. Most people don’t even know what CYP450 enzymes are. You’re playing Russian roulette with your hepatocytes. I’ve read the journals. You haven’t. So stop pretending you understand this.
siva lingam
February 1, 2026 AT 03:13so u saying i cant take tylenol after beer? lmao