Analgesic Nephropathy: How NSAIDs Damage Kidneys and What to Use Instead
 Jan, 9 2026
Jan, 9 2026
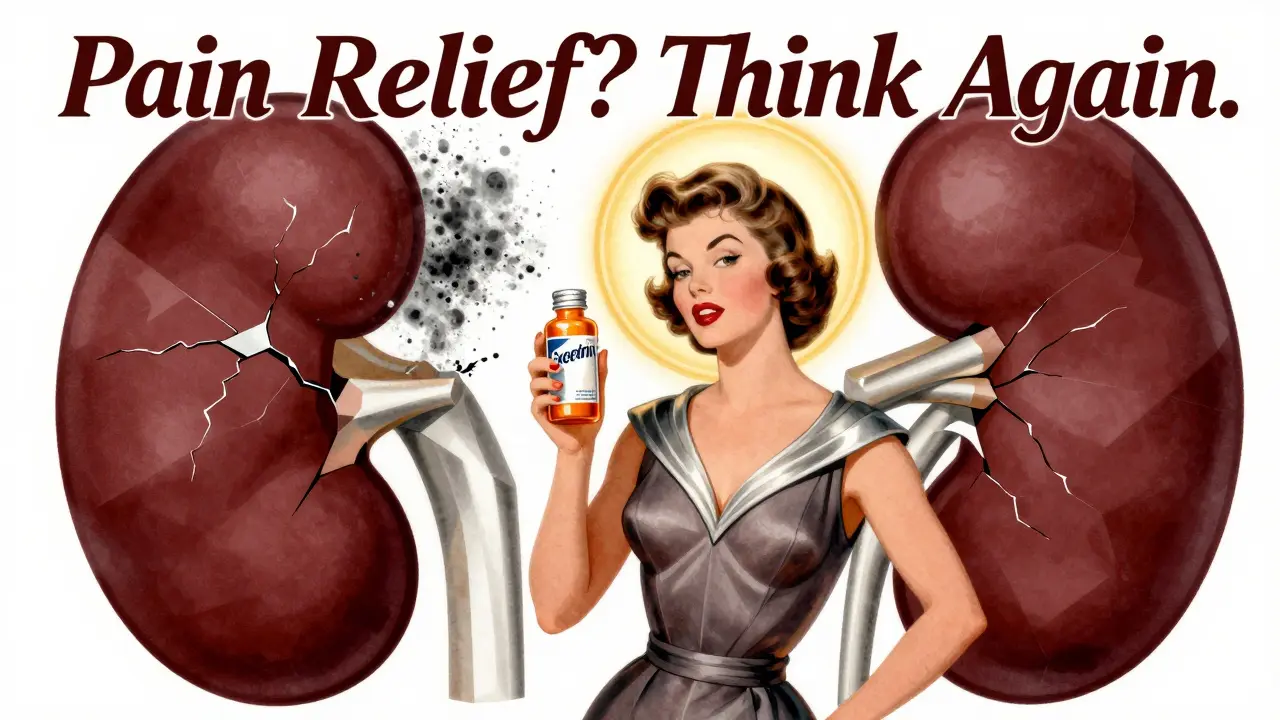
For years, millions of people have reached for over-the-counter painkillers like ibuprofen, naproxen, or Excedrin without a second thought. They’re cheap, easy to get, and seem harmless. But what if taking just a few pills a day for years is quietly damaging your kidneys? That’s the reality of analgesic nephropathy-a preventable form of chronic kidney disease caused by long-term, high-dose use of common pain medications.
What Exactly Is Analgesic Nephropathy?
Analgesic nephropathy isn’t a sudden injury. It’s a slow, silent breakdown of the kidneys caused by years of heavy painkiller use. The damage happens in the inner part of the kidney-the tubules and interstitial tissue-that filters waste and balances fluids. Over time, these tiny structures scar and die, reducing the kidney’s ability to function.
It’s not just one drug. The condition is tied to long-term use of NSAIDs (like aspirin, ibuprofen, and naproxen) and acetaminophen, especially when taken in combination. Back in the 1970s and 80s, many pain relievers contained phenacetin-a now-banned ingredient that was especially hard on the kidneys. Today, the main culprits are over-the-counter combo pills: Excedrin, Goody’s Powder, and similar products that mix acetaminophen, aspirin, and caffeine. These are the most dangerous because they encourage higher daily doses.
People who take six or more pills a day for three years or more are at the highest risk. And while men are affected, women make up 72% of diagnosed cases-often because they’re managing chronic headaches, menstrual pain, or arthritis with daily pills.
How Do These Painkillers Actually Hurt Your Kidneys?
NSAIDs work by blocking enzymes that cause inflammation and pain. But those same enzymes also help keep blood flowing to your kidneys. When you take them daily, your kidneys get less blood. That’s not a problem for a healthy person taking one pill now and then. But over months and years, that reduced blood flow causes oxygen starvation in kidney tissue. The cells start to die.
At the same time, these drugs deplete antioxidants in the kidneys, leaving them vulnerable to oxidative stress. Think of it like rusting from the inside. The damage starts in the renal papillae-the cone-shaped tips of the kidney’s inner structures. These can begin to die off, a process called papillary necrosis. Eventually, the kidney tissue becomes scarred and stiff, leading to chronic interstitial nephritis.
The worst part? You won’t feel it until it’s advanced. Early stages show no symptoms. No pain. No swelling. Just a slow, silent drop in kidney function. That’s why routine blood tests are critical.
Who’s Most at Risk?
It’s not just people who take drugs illegally or in massive doses. The typical patient is a woman over 45 who’s been managing daily pain for years. Maybe it’s migraines, arthritis, or back pain. She takes 2-3 pills every day because it works. She doesn’t think of it as medicine-just a way to get through the day.
Other high-risk groups include people with:
- High blood pressure
- Diabetes
- Existing chronic kidney disease
- Heart failure or liver disease
- Age over 60
Even if you don’t have these conditions, taking NSAIDs more than 3 days a week for over a year raises your risk. And if you’re using combo pills with caffeine or codeine, your risk jumps 3.7 times higher than with single-ingredient painkillers.

How Is It Diagnosed?
Because there are no early symptoms, diagnosis often happens by accident-during a routine blood test that shows elevated creatinine or a drop in GFR (glomerular filtration rate). A GFR below 60 for three months means kidney damage is present.
Other signs include:
- Non-nephrotic proteinuria (small amounts of protein in urine, under 3.5 grams/day)
- Bland urinary sediment (no red or white blood cells)
- Sterile pyuria (white blood cells in urine without infection)
- High blood pressure that’s hard to control
- Anemia not explained by other causes
The best imaging test is a noncontrast CT scan. It can show calcifications in the renal papillae with 87% sensitivity and 97% specificity. That’s rare for a kidney condition-it’s one of the few where imaging gives a clear, unmistakable signal.
In January 2023, the FDA approved the first point-of-care urine test called NephroCheck. It detects early signs of renal papillary damage with 92% accuracy. This is a game-changer for catching the disease before it’s too late.
What Happens If You Don’t Stop?
If you keep taking high doses of NSAIDs or combo analgesics, the damage keeps building. By the time symptoms show up, you’re already in advanced stages:
- Flank pain or blood in urine
- Passing pieces of dead kidney tissue (renal papillae)
- Urinary tract blockages
- Severe anemia
- Fluid retention and swelling
Eventually, the kidneys fail. About 2-3% of all chronic kidney disease cases in the U.S. are caused by analgesic nephropathy-that’s 15,000 to 20,000 new cases every year. And once you reach end-stage renal disease, you need dialysis or a transplant. The annual cost for dialysis? Around $90,000 per person.
But here’s the good news: if caught early, the damage can stop.
Stopping NSAIDs Doesn’t Mean Stopping Pain Relief
Many patients panic when told to stop their painkillers. They worry they’ll be stuck in pain with no alternatives. That’s not true. There are safer, effective ways to manage chronic pain.
1. Switch to topical NSAIDs. Gels, patches, or creams like diclofenac gel reduce systemic exposure by 90%. A 2021 study showed they work just as well as oral pills for joint pain-with zero decline in kidney function after 12 weeks.
2. Use heat therapy. Devices like ThermaCare HeatWraps reduce osteoarthritis pain by 40-60%. No drugs. No side effects. Just steady, soothing heat that loosens stiff muscles and joints.
3. Try physical therapy and movement. The American College of Rheumatology recommends trying physical therapy for 4-6 weeks before even considering daily painkillers. Strengthening muscles around painful joints reduces strain and pain naturally.
4. Consider cognitive behavioral therapy (CBT). Chronic pain changes how your brain processes signals. CBT helps retrain that response. Studies show it reduces pain perception as effectively as some medications-with no risk to your kidneys.
5. For migraines: CGRP inhibitors. Prescription drugs like Aimovig or Emgality block migraine triggers without touching the kidneys. They cost $650 a month, but they’re the only truly kidney-safe option for frequent migraines.
And yes, acetaminophen is safer than NSAIDs-but not risk-free. Taking more than 3,000 mg a day for five years increases your risk of chronic kidney disease by 68%. The FDA’s limit? 3,000 mg daily. Not 4,000. Not 5,000. 3,000.

What Should You Do Now?
If you’ve been taking NSAIDs or combo painkillers regularly, here’s what to do:
- Count your pills. How many NSAIDs or acetaminophen pills do you take per week? If it’s more than 3 days, you’re in the danger zone.
- Check your labels. Are you using combo products? If they list caffeine, codeine, or multiple active ingredients, stop. Switch to single-ingredient versions.
- Get a blood test. Ask your doctor for a serum creatinine and estimated GFR. Do it now-don’t wait for symptoms.
- Start alternatives. Try topical NSAIDs, heat therapy, or physical therapy this week. Don’t wait to quit painkillers cold turkey-replace them first.
- Set limits. Never take NSAIDs for more than 10 days in a row without seeing a doctor. And never exceed 3,000 mg of acetaminophen daily.
One patient on Reddit shared: ‘I took 8-10 Excedrin Migraine tablets daily for 7 years before my GFR dropped to 45. My nephrologist said I was lucky it wasn’t worse-many people need dialysis from this.’
But another study found that 73% of patients who stopped analgesics early saw their kidney function stabilize. No decline. No dialysis. Just stopping the damage.
Why This Matters More Than Ever
A 2023 CDC report found that 41% of American adults still exceed recommended NSAID doses. Among people with chronic pain, that number jumps to 67%. Meanwhile, the FDA has updated labels to warn about kidney risks, and manufacturers have started reducing caffeine in combo pills. But awareness is still low.
Most patients don’t believe over-the-counter drugs can cause kidney damage. A Cedars-Sinai survey found 62% of people with analgesic nephropathy were shocked when they heard the diagnosis.
That’s the real problem-not the drugs themselves, but the myth that they’re harmless. Painkillers aren’t candy. They’re powerful chemicals with serious side effects when used long-term.
By changing how you manage pain, you’re not giving up relief-you’re protecting your future. Your kidneys can’t regenerate. Once they’re scarred, the damage is permanent. But if you act now, you can stop it before it starts.
Can I still take ibuprofen for headaches?
Yes-but only occasionally. Limit ibuprofen to no more than 1,200 mg per day and no more than 3 days per week without talking to your doctor. For daily headaches, see a neurologist. There are better, kidney-safe treatments like CGRP inhibitors or preventive therapies that don’t rely on daily painkillers.
Is acetaminophen safe for my kidneys?
Acetaminophen is safer than NSAIDs, but it’s not risk-free. Taking more than 3,000 mg daily for five or more years increases your risk of chronic kidney disease by 68%. The FDA’s safe limit is 3,000 mg per day. Many people unknowingly exceed this by taking combo pills or multiple products with hidden acetaminophen.
What’s the best alternative to NSAIDs for arthritis pain?
Topical diclofenac gel is the top choice. It delivers pain relief directly to the joint with 90% less systemic absorption than pills. Heat wraps, physical therapy, and weight management also help. For moderate to severe arthritis, your doctor may recommend corticosteroid injections or newer biologic drugs that don’t harm the kidneys.
Can kidney damage from painkillers be reversed?
Early damage can stabilize and sometimes improve if you stop the painkillers and manage other risk factors like blood pressure and diabetes. But once scarring (fibrosis) sets in, it’s permanent. The goal isn’t to reverse damage-it’s to stop it before it starts.
How often should I get my kidney function checked if I take painkillers?
If you take NSAIDs or acetaminophen regularly (more than 3 days a week), get a blood test for creatinine and GFR every 6 months. If you have high blood pressure, diabetes, or existing kidney issues, check every 3 months during the first year. Early detection saves kidneys.
Are there any new painkillers that don’t hurt the kidneys?
Yes. CGRP inhibitors for migraines and topical NSAIDs are proven kidney-safe. CBD products show no kidney harm at doses under 1,500 mg/day, but evidence is still limited. Research is ongoing for new drugs like selepressin, which may protect kidneys during NSAID use. But for now, the safest option is reducing reliance on daily oral painkillers altogether.
Next Steps for People with Chronic Pain
If you’ve been taking painkillers daily for years, don’t panic-but don’t wait either. Start by switching from combo pills to single-ingredient acetaminophen or NSAIDs. Then, begin replacing one daily pill with a non-drug option: a heat wrap, a 15-minute walk, or a stretching routine. Track your pain and medication use in a journal. Schedule a blood test with your doctor. Talk about alternatives.
Your kidneys have been working for you every minute of every day. They don’t ask for much. But they need you to protect them-not just from disease, but from the very things you use to feel better.
Jaqueline santos bau
January 11, 2026 AT 20:10Okay but like… I’ve been taking 8 Excedrin a day for 10 years and my kidneys are fine. I’m 52, run marathons, and my doctor says I’m ‘low-risk.’ Who are you to tell me what my body can handle? 😏
chandra tan
January 11, 2026 AT 20:35Bro in India we don’t even know what NSAID means. We just take painkillers like candy. My aunty takes 5 paracetamol before breakfast for her back pain. She’s 70 and still dancing at weddings. Maybe the real problem is overthinking? 🤷♂️
Dwayne Dickson
January 12, 2026 AT 12:06While the clinical presentation of analgesic nephropathy is well-documented in the literature, the author’s conflation of epidemiological risk factors with prescriptive behavioral mandates lacks nuance. The renal tubulointerstitial injury cascade, mediated by prostaglandin suppression and oxidative stress, is indeed dose- and duration-dependent-but individual pharmacokinetic variability, comorbidities, and genetic polymorphisms (e.g., CYP2E1, GSTM1) significantly modulate susceptibility. A blanket ‘stop all NSAIDs’ directive ignores the risk-benefit calculus for patients with refractory pain. Evidence-based harm reduction, not moralizing, should guide clinical discourse.
Mario Bros
January 13, 2026 AT 18:56Bro I was literally this person. Took 6 Excedrin a day for 5 years. My GFR dropped to 51. I switched to topical diclofenac + heat wraps. Now my GFR’s back to 72. No dialysis. No trauma. Just stopped being dumb. 🙏 You got this.
Jake Nunez
January 14, 2026 AT 00:50Topical NSAIDs are great, but they don’t work for migraines. I tried them. Zero effect. I still need the oral stuff. And yeah, I know I shouldn’t, but I do. What’s the alternative? Just suffer? That’s not a solution, that’s punishment.
Michael Marchio
January 15, 2026 AT 19:05Let’s be honest: this isn’t about kidneys. It’s about control. The medical-industrial complex wants you to believe that your pain is a problem to be managed with their expensive, patented solutions-CGRP inhibitors at $650 a month, physical therapy appointments, CBT sessions. Meanwhile, your $5 bottle of Excedrin has been working for decades. The real danger isn’t the drug-it’s the guilt-tripping, fear-mongering, ‘you’re slowly dying’ narrative pushed by people who profit from your anxiety. Don’t let them make you feel bad for taking what works. Your body, your choice.
Jake Kelly
January 15, 2026 AT 22:07I appreciate the effort to raise awareness. I’ve seen too many people ignore this until it’s too late. If you’re reading this and you’ve been taking daily painkillers-please, just get a simple blood test. It takes five minutes. You might save your kidneys. No judgment, just care.
Paul Bear
January 16, 2026 AT 00:24Correction: the FDA’s safe limit for acetaminophen is 3,250 mg/day for immediate-release formulations, not 3,000 mg. The 3,000 mg recommendation is an advisory from the American Liver Foundation for high-risk populations, not a regulatory limit. Also, the 68% increased risk figure cited is from a 2017 observational study with significant confounding variables (e.g., BMI, alcohol use, polypharmacy). Correlation ≠ causation. And for the record, ‘renal papillary necrosis’ is not visible on noncontrast CT in 87% of cases-it’s detectable in 87% of *confirmed* cases, which is a different statistical category entirely. Please cite sources properly.
Kunal Majumder
January 17, 2026 AT 02:10My dad had kidney issues from painkillers. He switched to yoga and turmeric paste. Now he walks 10 km every morning. No pills. No problems. You don’t need chemicals to feel better. Your body’s smarter than you think.
Aurora Memo
January 17, 2026 AT 10:08Thank you for sharing this. I’m a nurse and I’ve seen too many patients come in with advanced kidney damage because they thought ‘it’s just a painkiller.’ I wish more people knew how silent this damage is. If you’re reading this and you’ve been taking daily pills-please, talk to someone. You don’t have to do it alone.