Antibiotics and Myasthenia Gravis: Risks, Safe Choices, and What to Watch For
 Feb, 4 2026
Feb, 4 2026
Antibiotics for Myasthenia Gravis Safety Checker
Check Your Antibiotic Safety
Select an antibiotic to see its risk level for myasthenia gravis patients and get safety recommendations.
Safety Information
Emergency Alert
Report to emergency services immediately if you experience:
- Difficulty breathing or swallowing
- Sudden muscle weakness in arms or legs
- Worsening drooping eyelids
For people with myasthenia gravis (MG), taking antibiotics isn't as simple as it seems-some can trigger dangerous muscle weakness. Understanding the risks of antibiotics myasthenia gravis is crucial for safe treatment.
Myasthenia Gravis is a rare autoimmune disorder where the body's immune system attacks the connection between nerves and muscles. It affects about 20 out of every 100,000 people in the United States. Symptoms include drooping eyelids, blurred vision, weakness in arms or legs, trouble chewing or swallowing, and breathing difficulties. This happens because the immune system damages acetylcholine receptors at the neuromuscular junction, making it harder for nerves to signal muscles properly.Why Antibiotics Can Worsen MG Symptoms
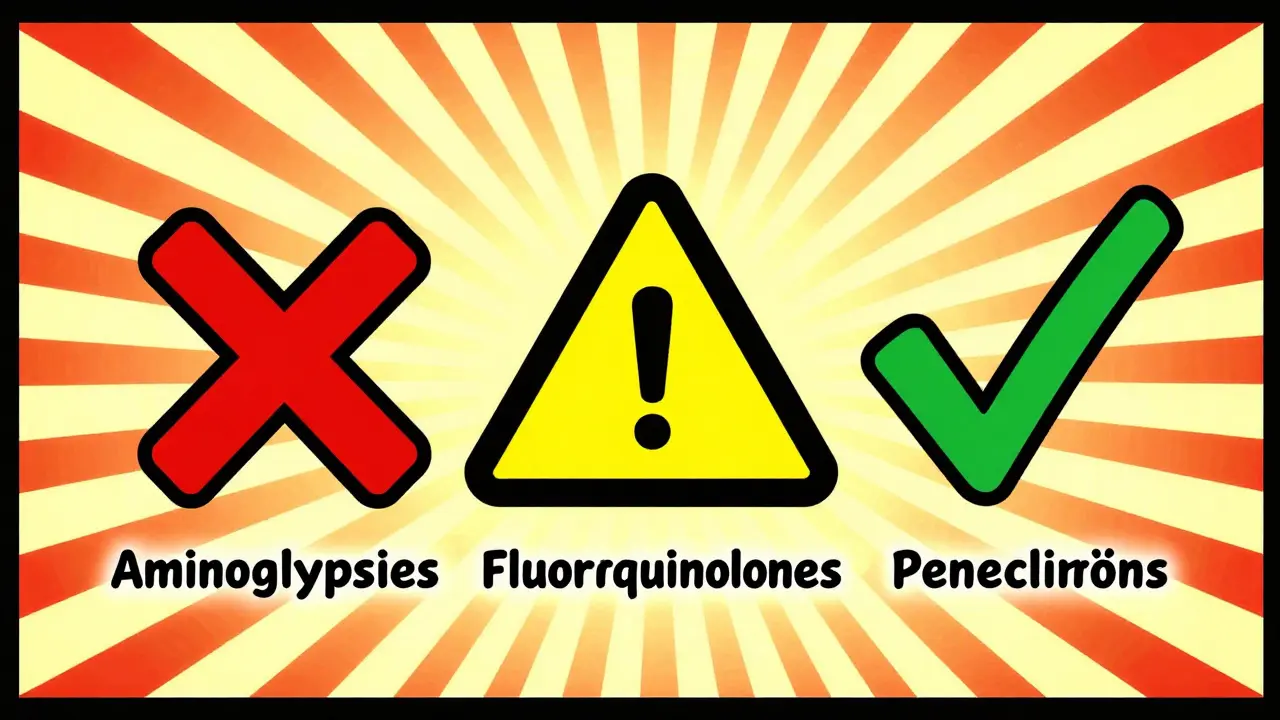
Antibiotics treat infections, but some can worsen MG symptoms. In MG, there are already fewer acetylcholine receptors. Certain antibiotics interfere with nerve-muscle communication further. This can lead to sudden muscle weakness or even a life-threatening myasthenic crisis where breathing becomes impossible. The FDA has issued black box warnings for specific antibiotics like fluoroquinolones and telithromycin due to these risks.
| Antibiotic Class | Risk Level | Common Examples | Notes |
|---|---|---|---|
| Fluoroquinolones | Moderate | Ciprofloxacin, Levofloxacin, Moxifloxacin | 2.4% risk for ciprofloxacin; FDA black box warning but newer data shows risk is lower than previously believed |
| Macrolides | Moderate | Azithromycin, Erythromycin | 1.5% exacerbation rate; Cleveland Clinic study found similar risk to penicillins |
| Aminoglycosides | High | Gentamicin, Tobramycin | Strong neuromuscular blocking effects; generally avoided in MG patients |
| Penicillins | Low | Amoxicillin, Penicillin V | 1.3% exacerbation rate; considered safest option for many infections |
| Tetracyclines | Intermediate | Doxycycline, Minocycline | Use with caution; may require monitoring for MG symptoms |
What Research Tells Us About Antibiotic Risks
A 2024 Cleveland Clinic study analyzed 365 MG patients and 918 antibiotic episodes. It found that about 2% of MG patients experienced worsening symptoms after taking antibiotics. However, the risk varies greatly by class. Penicillins like amoxicillin had only a 1.3% exacerbation rate-lower than fluoroquinolones (2.4% for ciprofloxacin) and macrolides (1.5%). Aminoglycosides remain the highest-risk group due to their direct blocking effect on muscle receptors.
Interestingly, infection itself was the main cause of symptom worsening in 88.2% of cases. This means treating infections quickly is often more critical than avoiding antibiotics. The study also found specific patient factors increase risk: recent hospitalization for MG, female sex, and diabetes. For example, women with MG have a 2.3 times higher chance of complications from antibiotics compared to men.
Which Antibiotics Are Safest for MG Patients?
When possible, doctors recommend penicillins like amoxicillin or penicillin V. These have the lowest risk of triggering MG flare-ups. For common infections like sinusitis or urinary tract infections, amoxicillin is often the best choice. If you need antibiotics for a bacterial infection, always ask your doctor: "Is there a safer option for my MG?"
Fluoroquinolones (like ciprofloxacin) and macrolides (like azithromycin) carry moderate risk. The FDA previously issued black box warnings for these, but recent research shows the actual danger is lower than once thought. Still, they should only be used when no safer alternatives exist. Aminoglycosides (like gentamicin) are generally avoided entirely in MG patients due to their high risk of causing severe weakness.
How to Stay Safe When Taking Antibiotics
Here’s what to do if you have MG and need antibiotics:
- Tell every doctor you see that you have MG before they prescribe anything. Write "MG" on your prescription bottle if possible.
- Ask if there’s a safer antibiotic option for your infection. For example, amoxicillin instead of ciprofloxacin for a urinary tract infection.
- Monitor for worsening symptoms during the first 72 hours of treatment. Watch for trouble breathing, swallowing, or new weakness in arms/legs.
- Keep emergency contact numbers for your MG specialist handy. Call immediately if symptoms worsen rapidly.
- Share your full medication list with pharmacists. They can flag potential risks before you pick up your prescription.
Frequently Asked Questions
Can antibiotics cause myasthenia gravis flare-ups?
Yes, certain antibiotics can trigger MG flare-ups by worsening neuromuscular weakness. However, not all antibiotics carry the same risk. Penicillins like amoxicillin have the lowest risk (1.3% exacerbation rate), while aminoglycosides like gentamicin are high-risk. Recent research shows the overall risk is lower than previously thought, but it's still important to choose antibiotics carefully.
Which antibiotics should MG patients avoid completely?
Aminoglycosides (gentamicin, tobramycin) are generally avoided entirely due to their strong neuromuscular blocking effects. Telithromycin (a macrolide) is absolutely contraindicated with a black box warning from the FDA. Fluoroquinolones and other macrolides should be used only when no safer alternatives exist, and only with close monitoring.
Why do some antibiotics worsen MG symptoms?
Antibiotics like aminoglycosides can directly block acetylcholine receptors at the neuromuscular junction. Others, like fluoroquinolones, may interfere with calcium channels needed for nerve signaling. In MG patients who already have fewer receptors, this extra interference can cause sudden muscle weakness or breathing trouble.
Should I stop taking antibiotics if I have MG?
Never stop prescribed antibiotics without talking to your doctor. Untreated infections can be life-threatening and often trigger MG exacerbations themselves. The key is to work with your specialist to choose the safest antibiotic for your specific infection and MG status. For example, amoxicillin is usually safe for common infections.
What should I do if my MG symptoms worsen while on antibiotics?
Seek emergency care immediately if you experience trouble breathing, swallowing, or sudden weakness in limbs. Call your MG specialist right away. They may adjust your treatment or give medications like intravenous immunoglobulin (IVIG) to quickly reverse the worsening symptoms. Always keep emergency contacts for your MG care team accessible.
Katharine Meiler
February 4, 2026 AT 19:25Based on the Cleveland Clinic's 2024 study of 365 MG patients, penicillins like amoxicillin have a 1.3% exacerbation rate, significantly lower than fluoroquinolones (2.4%). However, newer data suggests fluoroquinolone risks may be lower than FDA's black box warning indicates. Still, individual factors like recent hospitalization or diabetes increase susceptibility. Always discuss antibiotic options with your neurologist before starting treatment.
Danielle Vila
February 5, 2026 AT 00:26Big Pharma is hiding the truth about antibiotics and MG. The FDA's black box warnings are just a cover-up. I've heard of people who died from antibiotics prescribed for MG. They want us to stay sick so we keep buying meds. Wake up, people!
Matthew Morales
February 5, 2026 AT 12:19bro i had a bad reaction to cipro too 😔 my muscles were weak for days. always check with your doc before taking antibiotics for mg. trust me, it's worth it.
Georgeana Chantie
February 6, 2026 AT 15:16America should ban all antibiotics that affect MG. We don't need foreign-made drugs. Let's develop our own safe ones. Stop trusting the FDA!
Carol Woulfe
February 8, 2026 AT 12:05The FDA's warnings are woefully inadequate. The true extent of antibiotic risks for MG patients is being deliberately obscured by pharmaceutical conglomerates. Only those with access to elite medical journals understand the gravity of this situation. The data is clear but suppressed for profit.
Kieran Griffiths
February 8, 2026 AT 22:48Let's keep it real-antibiotics are necessary for infections, but choosing the right one matters. Penicillins are generally safe, but always communicate with your specialist. Ignoring the risks isn't helpful; informed decisions are.
Tehya Wilson
February 10, 2026 AT 02:36Antibiotics dangerous for MG. Avoid all.
Brendan Ferguson
February 11, 2026 AT 10:51Based on current evidence, penicillins like amoxicillin are indeed the safest option for most infections in MG patients. However, each case is unique and requires careful consideration. For instance, a urinary tract infection might necessitate a different approach than a sinus infection. It's also important to note that individual factors such as recent hospitalization, diabetes status, and sex can influence the risk of exacerbation. Women with MG have a 2.3 times higher chance of complications from antibiotics compared to men, according to recent studies. Additionally, the Cleveland Clinic's 2024 research found that infection itself is the main cause of symptom worsening in 88.2% of cases, which underscores the importance of timely treatment. While fluoroquinolones and macrolides carry moderate risk, they should only be used when safer alternatives aren't available. Aminoglycosides should generally be avoided entirely due to their strong neuromuscular blocking effects. Always share your full medication list with your pharmacist and healthcare team to avoid potential interactions. Remember, the key is to work closely with your specialists to find the safest treatment path for your specific situation. Don't hesitate to ask questions or seek second opinions if needed. Your health is worth the extra effort. In my own experience managing MG, I've found that clear communication with my neurologist has been crucial in avoiding complications from necessary medications. It's also important to monitor for symptoms like sudden weakness or breathing difficulties during antibiotic treatment and seek immediate care if they arise. Collaboration between patient and provider is the best way to navigate these risks safely.
jan civil
February 12, 2026 AT 04:29How do aminoglycosides block acetylcholine receptors? Is it through direct binding or another mechanism?
Jennifer Aronson
February 12, 2026 AT 10:48The mechanism involves aminoglycosides binding to the neuromuscular junction's acetylcholine receptors, inhibiting nerve signal transmission. This is particularly dangerous for MG patients with already reduced receptor density. However, each case varies-consulting a specialist is essential.
Kate Gile
February 13, 2026 AT 01:14Knowledge is power! Understanding how aminoglycosides affect receptors helps us make safer choices. Always share your full medication history with doctors and pharmacists. Together we can navigate MG treatment safely-stay informed and advocate for yourself!