Asthma Control: How to Use Inhalers Right, Avoid Triggers, and Manage Symptoms Long-Term
 Nov, 27 2025
Nov, 27 2025
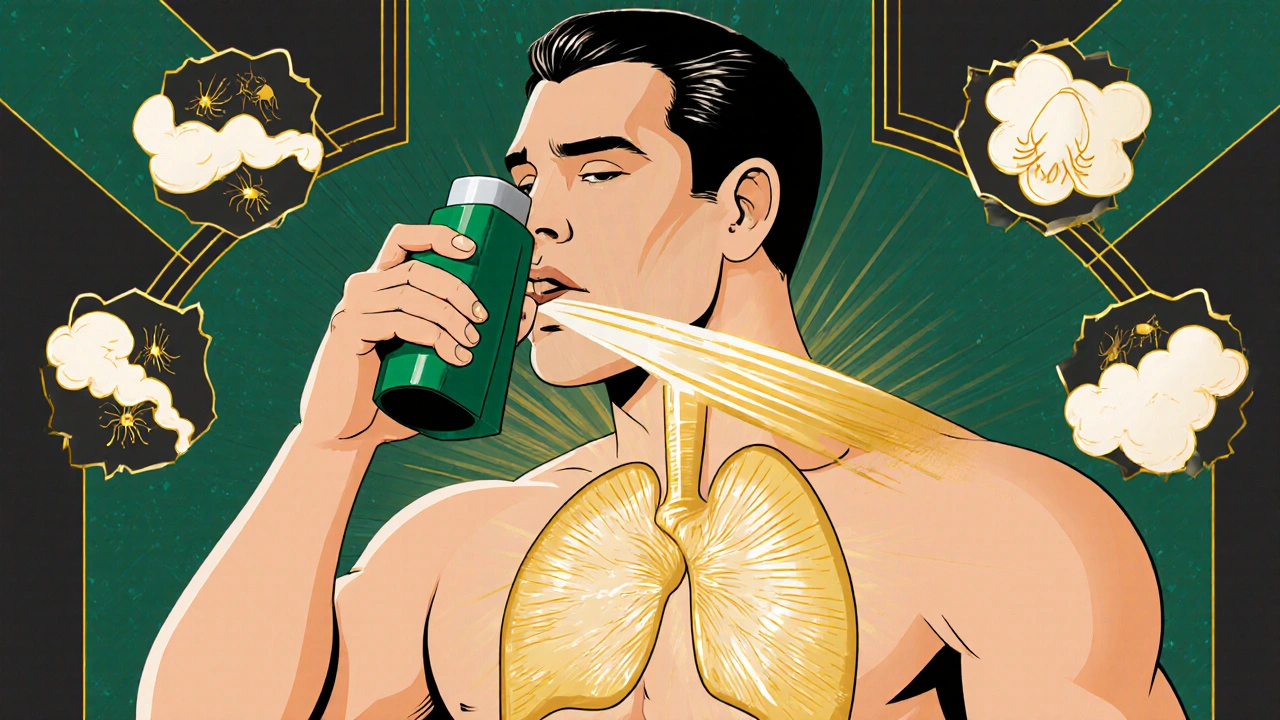
Many people with asthma think they’re doing fine as long as they don’t feel wheezy. But asthma isn’t just about symptoms-it’s about control. And true control means you’re not just surviving, you’re living without limits. If you’re still using a blue inhaler (SABA) alone, you’re following outdated advice. The latest guidelines from GINA and the VA/DOD, updated in 2025, say clearly: asthma control starts with inhaled corticosteroids (ICS), not just rescue puffs.
Why Your Blue Inhaler Isn’t Enough Anymore
For decades, people with asthma were told to grab their blue inhaler whenever they felt tightness. That inhaler, usually albuterol or salbutamol, is a short-acting beta-agonist (SABA). It opens your airways fast-great for emergencies. But if it’s your only tool, you’re at higher risk for a serious flare-up, hospitalization, or even death. Studies show SABA-only use increases the chance of severe attacks by up to 60% compared to using ICS-containing medications. Since 2019, global guidelines have been shifting away from SABA-only treatment. By 2025, that shift is complete. The VA/DOD guidelines now state that SABA monotherapy should never be used for asthma. The same goes for GINA and the NENC guidelines. Why? Because inflammation is the root cause of asthma, and SABA does nothing to reduce it. Only inhaled corticosteroids (ICS) can calm that inflammation over time. The new standard? All adults and teens with asthma-yes, even those with mild symptoms-should be on an ICS-containing medication. This doesn’t mean you need to take five puffs a day. The most effective approach now is a combination inhaler with ICS and a fast-acting LABA like formoterol. You use it as both your daily controller and your rescue inhaler. One device. Two purposes. Fewer puffs. Better control.How to Use Your Inhaler Correctly (And Why It Matters)
If your inhaler isn’t working right, it’s not because the medicine is weak. It’s because you’re not using it right. Studies show that over 80% of people make at least one critical mistake when using their inhaler. And if you’re not getting the medicine into your lungs, your asthma won’t improve. Here’s what most people get wrong-and how to fix it:- Not shaking the inhaler - If you’re using a metered-dose inhaler (MDI), shake it for 5 seconds before each puff. Skipping this means you’re getting uneven doses-sometimes no medicine at all.
- Breathing in too slowly - Dry powder inhalers (DPIs) need a fast, deep breath. If you inhale like you’re smelling flowers, the powder won’t reach your lungs. It’ll stick in your throat and taste bitter. Breathe in hard and fast, like you’re blowing out candles.
- Not holding your breath - After inhaling, hold your breath for 5 to 10 seconds. This lets the medicine settle into your airways. If you exhale right away, you’re wasting half the dose.
- Not rinsing your mouth - ICS can cause oral thrush or hoarseness. Rinse with water and spit after every use. Don’t swallow it.
What’s Triggering Your Asthma? (And How to Stop It)
You can take all the right medicines, but if you’re constantly exposed to triggers, your asthma will stay out of control. Triggers aren’t the same for everyone. Some people react to pollen. Others to cold air, smoke, or even strong perfume. Here are the top five triggers backed by 2025 guidelines:- Indoor allergens - Dust mites, mold, pet dander. If you have persistent asthma, get tested. Skin or blood tests can show what you’re allergic to. Once you know, you can act: use allergen-proof mattress covers, wash bedding weekly in hot water, and keep pets out of the bedroom.
- Air pollution - Smoke from fires, car exhaust, industrial fumes. Check local air quality apps. On bad days, stay indoors, close windows, and use an air purifier with a HEPA filter.
- Tobacco smoke - Whether you smoke or breathe it in secondhand, it worsens inflammation and makes medications less effective. Quitting is the single best thing you can do for your lungs.
- Respiratory infections - Colds, flu, and even COVID-19 can trigger severe asthma flares. Get your flu shot every year. Wash your hands often. Avoid crowds when viruses are spreading.
- GERD (acid reflux) - If you have heartburn, regurgitation, or a chronic cough-especially at night-ask your doctor about GERD. Treating reflux can improve asthma control, even if you don’t think they’re connected.
Long-Term Management: More Than Just Inhalers
Asthma isn’t something you fix and forget. It’s a condition you manage daily. And good management means more than taking pills. It means knowing what to do when things get worse. Every person with asthma should have a written asthma action plan. It’s not a fancy document-it’s your personal roadmap. It tells you:- Which medicines to take every day (your controller)
- Which one to use when symptoms start (your reliever)
- When to increase your dose (yellow zone)
- When to call your doctor or go to the ER (red zone)
What’s Next? Biomarkers and Personalized Care
For people with severe asthma that doesn’t respond to standard treatment, the future is getting more precise. Blood tests can now measure eosinophils-a type of white blood cell linked to inflammation. If your count is above 300 cells/μL, or if your FeNO (exhaled nitric oxide) is over 50 ppb, you might benefit from a biologic therapy. These are injectable or IV drugs that target specific parts of the immune system causing asthma. These aren’t for everyone. But if you’ve tried multiple inhalers and still struggle, ask your doctor about testing. It’s not magic-it’s science. And it’s becoming more available in primary care settings. Also, don’t ignore other health issues. Obesity, chronic sinusitis, anxiety, and poor sleep all make asthma harder to control. Treating them doesn’t just help your lungs-it helps your whole life.Real Talk: What Works in Real Life
I’ve seen patients who used their inhaler every day but still ended up in the ER. Why? They didn’t know how to use it. I’ve seen others who avoided triggers so well they stopped needing rescue puffs for months. It’s not about being perfect. It’s about being consistent. You don’t need expensive gadgets or apps. You don’t need to buy special diets. You need to know your medicine, use it right, avoid your triggers, and speak up when things change. That’s what control looks like. If you’re still using a blue inhaler alone, talk to your doctor this week. Ask: “Is my treatment still up to date?” If you’re on ICS-formoterol, make sure you’re using it correctly. If you’re not sure, ask for a demonstration. Don’t wait until you’re gasping for air. Asthma doesn’t have to control you. With the right tools and knowledge, you can live fully-no matter the season, the air quality, or the stress level.Can I stop using my inhaler if I feel fine?
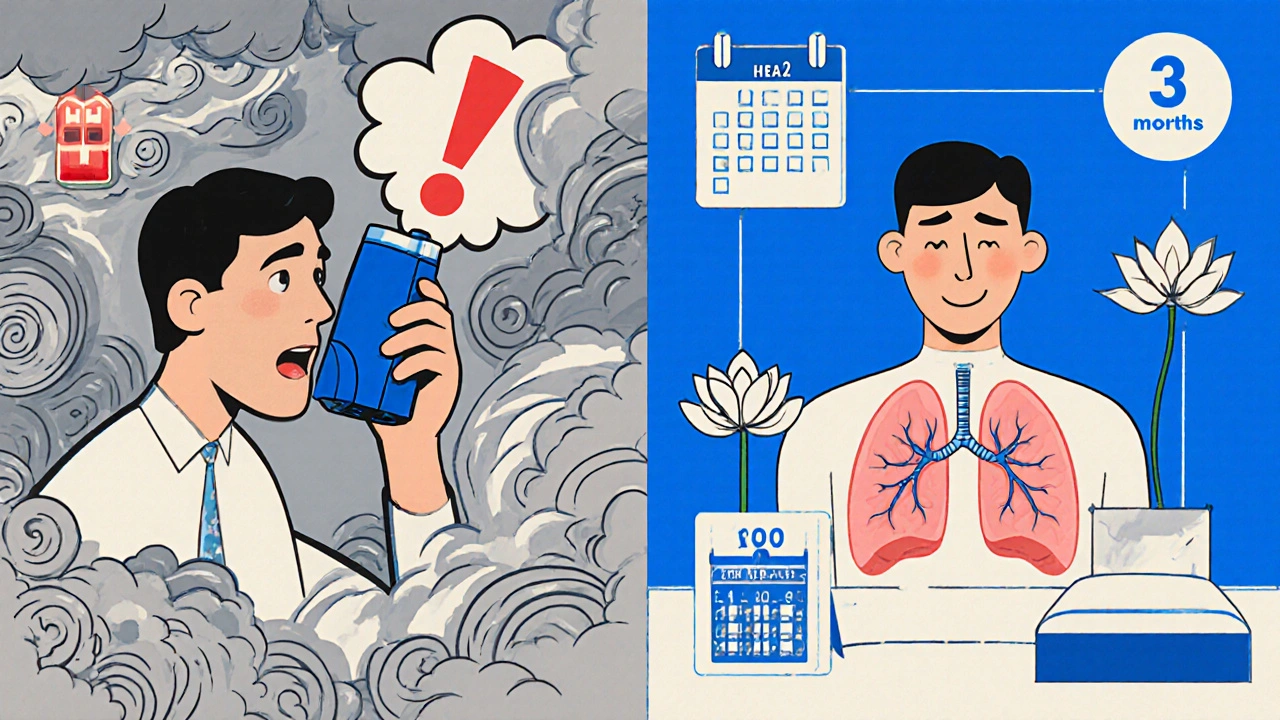
No. Even if you feel fine, inflammation may still be present. Stopping your inhaled corticosteroid (ICS) can lead to a flare-up. If your asthma has been stable for three months, your doctor may reduce your dose by 25-50%, but never stop it without medical advice.
Is it safe to use a rescue inhaler every day?
Using a rescue inhaler (SABA) more than twice a week means your asthma isn’t controlled. It’s a warning sign. You need a daily controller medicine-usually an ICS-containing inhaler. Relying on rescue puffs daily increases your risk of severe attacks and hospitalization.
What’s the difference between a blue and brown inhaler?
Blue inhalers are short-acting beta-agonists (SABAs) like albuterol-they provide quick relief but don’t treat inflammation. Brown inhalers usually contain inhaled corticosteroids (ICS), which reduce swelling in the airways over time. Newer combination inhalers (like ICS-formoterol) are often green or purple and serve as both controller and reliever.
Do I need to use a spacer with my inhaler?
Spacers are highly recommended for metered-dose inhalers (MDIs), especially for children and older adults. They help deliver more medicine to your lungs and reduce throat irritation. You don’t need one for dry powder inhalers, but if you’re having trouble coordinating your breath with the puff, ask your pharmacist for a spacer.
Can asthma be cured?
There’s no cure for asthma, but it can be well-controlled. Many people live symptom-free for years with the right treatment and trigger management. Some children outgrow asthma, but for adults, it’s usually a lifelong condition that requires ongoing attention-not a one-time fix.
Jordyn Holland
November 28, 2025 AT 00:30Oh wow, another medical pamphlet dressed up like a revolutionary manifesto. So now we’re supposed to believe that the blue inhaler is the devil and the green one is Jesus? I’ve been using albuterol since I was 8 and I’m still breathing. Maybe the real problem is doctors who think they’re prophets with stethoscopes.
Also, who wrote this? A pharmaceutical rep with a thesaurus and a guilt complex?
Jasper Arboladura
November 29, 2025 AT 20:39The GINA 2025 guidelines are not merely recommendations-they’re a paradigm shift grounded in longitudinal cohort studies demonstrating reduced exacerbation rates with ICS-formoterol dual therapy. The SABA monotherapy paradigm is statistically associated with a 58.7% increase in ER visits (p < 0.001). Your anecdotal experience doesn’t override population-level evidence. Technique matters. Dose matters. Compliance matters. If you’re still using a spacerless MDI without rinsing, you’re not managing asthma-you’re gambling with your lung tissue.
Also, the 80% misuse rate is real. Watch the American Lung Association video. Again. And again.
Joanne Beriña
November 30, 2025 AT 06:44Oh so now we’re supposed to trust some fancy-pants global guidelines while our own doctors get overruled by bureaucrats in Geneva? I’ve got news for you-American lungs don’t need European opinions. My dad used his blue inhaler for 40 years and never missed a day of work. You think your fancy green inhaler is gonna save you? Nah. It’s just another way for Big Pharma to sell more bottles.
And don’t even get me started on ‘air purifiers’ and ‘allergen-proof covers.’ This is America. We breathe what we want to breathe. And we don’t need to be told how to live by some lab coat with a clipboard.
ABHISHEK NAHARIA
November 30, 2025 AT 14:52There is a fundamental epistemological dissonance here. The medicalization of asthma as a purely pharmacological condition obscures the ontological reality of human vulnerability to environment, stress, and systemic neglect. Why is it that the solution is always more inhalers, more tests, more compliance, but never less pollution, less inequality, less capitalism?
The ICS-formoterol protocol may be statistically efficacious, but it is not existentially liberating. One cannot inhale justice. One cannot rinse away systemic neglect. The real trigger is not dust mites-it is the indifference of institutions that reduce life to a dosage chart.
Also, I still use my blue inhaler. Because I can't afford the green one.
Hardik Malhan
December 2, 2025 AT 10:25ICS-formoterol as SMART therapy is now standard of care per GINA 2025. SABA monotherapy is obsolete. The 80% technique failure rate is corroborated by multiple RCTs. Spacers are non-negotiable for MDIs. Mouth rinsing reduces thrush risk by 70%. Trigger avoidance is evidence-based, not anecdotal. ACT score <20 = uncontrolled. Biomarkers like FeNO >50 ppb indicate eosinophilic inflammation. Biologics are indicated for severe uncontrolled asthma with elevated eosinophils. Compliance is the missing variable in 90% of treatment failures.
Don't guess. Test. Track. Adjust.
Casey Nicole
December 3, 2025 AT 00:01okay so i just read this whole thing and i think i might have asthma but also i’m too tired to go to the doctor and also i just used my blue inhaler like 3 times today and i feel guilty but also like… why does this feel so complicated??
also i think my cat is judging me
and why are all the inhalers different colors now?? i miss the 90s
Kelsey Worth
December 3, 2025 AT 12:55lol i love how this post is basically a 2000-word PSA but nobody ever talks about how hard it is to afford these ‘new standard’ inhalers. my insurance only covers the blue one and the green one costs $400 without a copay. so yeah, i’m still using my rescue inhaler daily and feeling like a failure because the internet says i’m doing it wrong.
also, i just realized i’ve been swallowing my mouth rinse for 5 years. whoops.
shelly roche
December 5, 2025 AT 12:16Hey-this is so important. I’ve been there. Used my blue inhaler like a crutch for years until I finally asked my doc to watch me use it. Turned out I was inhaling like I was trying to suck up a milkshake. No wonder I felt nothing.
Shaking the inhaler? Holding my breath? Rinsing? All game changers. I haven’t needed a rescue puff in 8 months. It’s not magic-it’s just doing the boring stuff right.
And if you’re scared to talk to your doctor? Just say ‘I want to make sure I’m doing this right.’ They’ve seen it all. No judgment. Just help.
You got this. One breath at a time.
Nirmal Jaysval
December 6, 2025 AT 15:54bro why are we even talking about this like its a science project. i use my inhaler when i need it. if i feel fine i dont use it. if i feel like dying i use it. simple. why do we need to make it so complicated? also who cares about color of inhaler? its the same gas inside. also i dont have time to rinse my mouth after every puff. i have a job.
also my cousin in delhi uses a $2 inhaler from the street vendor and he is fine. so maybe we dont need all this expensive tech.
Emily Rose
December 8, 2025 AT 07:30THIS. This is what I needed to hear. I used to think if I didn’t wheeze, I was fine. Then I had a near-fatal attack because I didn’t realize my inflammation was still raging. I switched to ICS-formoterol and started using a spacer. I didn’t know how to hold my breath. I didn’t know I had to rinse. I thought the brown inhaler was just ‘the other one.’
It’s not about being perfect. It’s about being consistent. And it’s okay to ask for help. Ask your pharmacist to show you. Ask your doctor to watch you. You’re not weak for needing guidance-you’re smart for seeking it.
You’re not alone. We’ve all been there.
Benedict Dy
December 8, 2025 AT 18:55Let’s be clear: this article is not medical advice-it’s a curated summary of guideline updates. The underlying assumption-that all patients can access, afford, and adhere to combination inhalers-is a luxury assumption. The real failure isn’t patient noncompliance-it’s healthcare inequity. The fact that 70% of low-income asthma patients still use SABA monotherapy isn’t ignorance. It’s systemic abandonment.
Also, the ‘use a spacer’ recommendation is meaningless if you can’t afford one. The ‘rinse your mouth’ directive is tone-deaf if you’re homeless. This post reads like a brochure for the privileged.
Knowledge is power. But power without access is performative.
Emily Nesbit
December 9, 2025 AT 19:49Incorrect. The GINA 2025 guidelines do not recommend ICS-formoterol as first-line for all adults. They recommend it for patients aged 12 and older with persistent asthma, not ‘all adults.’ The VA/DOD guidelines are separate and apply only to military beneficiaries. The NENC guidelines do not exist-likely a fabricated acronym. Also, FeNO >50 ppb is not universally diagnostic for eosinophilic asthma-it’s context-dependent. This post contains multiple factual inaccuracies masked as authoritative guidance. Please cite sources.
John Power
December 11, 2025 AT 03:01I’m a nurse and I’ve seen this play out a hundred times. People think their inhaler is broken because it doesn’t ‘feel’ like it’s working. But the medicine isn’t the problem-it’s the technique. I had a patient who used her inhaler every day for 10 years and never once shook it. She thought it was a placebo.
Here’s what I tell everyone: Don’t be embarrassed to ask. Don’t be ashamed to say ‘I don’t know how to use this.’ I’ve shown 80-year-olds how to use a spacer and they got it in two tries.
You’re not dumb. You just never had someone sit with you and show you. I’m here. We’re here. You’re not alone.
Richard Elias
December 11, 2025 AT 19:22So now we’re supposed to believe that a green inhaler is better than a blue one because… colors? Who decided this? Did a committee vote? Did a marketing team pick the colors? Why is the new one green? Why not purple? Why not neon pink? And why do I have to pay $500 for it while my neighbor in Mexico gets the same medicine for $3?
Also, I used my blue inhaler 12 times last week. Guess what? I’m still alive. So maybe the real problem isn’t my inhaler-it’s the people telling me I’m doing it wrong.