Betapace (Sotalol) vs Other Anti‑Arrhythmic Drugs: A Comparison Guide
 Sep, 30 2025
Sep, 30 2025
Anti-Arrhythmic Drug Selector
This tool helps determine which anti-arrhythmic drug may be best suited for your condition based on key factors such as heart disease status, kidney function, and monitoring capability.
When treating irregular heartbeats, Betapace is the brand name for Sotalol, a classIII anti‑arrhythmic that also blocks beta‑adrenergic receptors. Patients often wonder if Betapace is the right choice or whether another drug might suit their condition better. This guide lays out the key facts, compares the most common alternatives, and helps you decide which option aligns with your health goals.
Quick Take
- Betapace combines classIII potassium‑channel blockade with beta‑blockade.
- It’s effective for atrial fibrillation and ventricular tachycardia but requires strict QT monitoring.
- Amiodarone offers broader rhythm control but carries long‑term organ toxicity.
- Dofetilide is another classIII agent, ideal for patients with heart failure who can tolerate hospitalization for initiation.
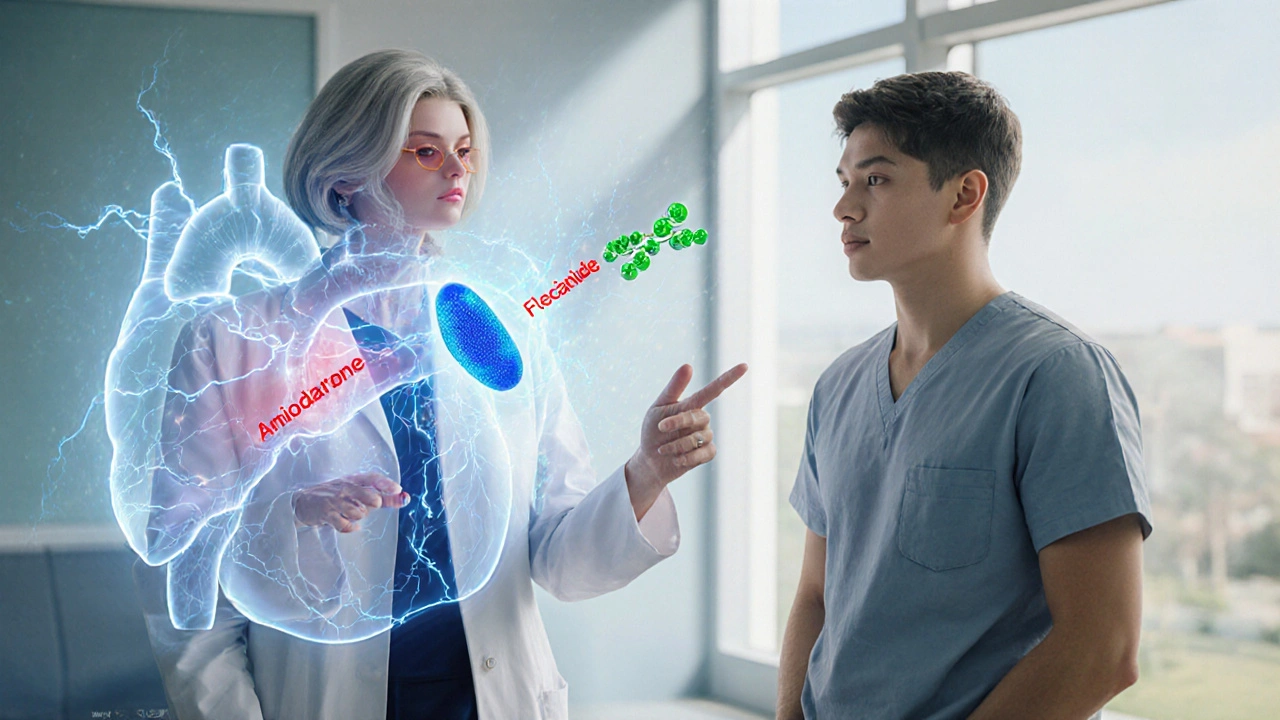
- Flecainide and Propafenone work as classIC agents; they’re excellent for “pill‑in‑the‑pocket” atrial fibrillation but are unsafe in structural heart disease.
How Betapace Works
Sotalol’s dual action sets it apart. As a Betapace tablet, it prolongs the cardiac action potential (classIII effect) while dampening sympathetic stimulation (beta‑blocker effect). Typical dosing starts at 80mg twice daily, titrating up to 160mg twice daily based on ECG‑derived QT intervals. Because QT prolongation can trigger torsades de pointes, clinicians check the QTc after the first dose, then daily for the first week.
Key side effects include fatigue, dizziness, and occasional bronchospasm in asthma patients. Since it lowers heart rate, patients with severe bradycardia should avoid Betapace. Drug interactions are common with other QT‑prolonging agents (e.g., certain antibiotics) and with medications that inhibit renal clearance, as sotalol is excreted unchanged by the kidneys.
Top Alternatives to Betapace
Below are the most frequently prescribed anti‑arrhythmics that clinicians consider when Betapace isn’t a perfect fit.
Amiodarone
Amiodarone is a classIII anti‑arrhythmic with a broad spectrum of action, affecting sodium, potassium, calcium channels and beta receptors. It’s often reserved for refractory atrial fibrillation or ventricular tachycardia. The usual loading dose is 800‑1200mg daily for 1‑2weeks, then a maintenance dose of 100‑200mg daily. While highly effective, long‑term use can damage the thyroid, lungs, liver, and skin. Regular lab monitoring (TSH, liver enzymes, chest X‑ray) is essential.
Dofetilide
Dofetilide is a pure classIII potassium‑channel blocker. It works well for patients with heart failure because it does not depress contractility. Initiation must occur in a hospital for four days of ECG monitoring; the dose is calculated from creatinine clearance (e.g., 500µg twice daily if CrCl > 60mL/min). Like Betapace, it risks QT prolongation, so careful dosing is critical.
Flecainide
Flecainide belongs to classIC, blocking fast sodium channels. It’s highly effective for “pill‑in‑the‑pocket” conversion of paroxysmal atrial fibrillation. A typical dose is 200‑300mg taken once during an episode. However, it should never be used in patients with coronary artery disease or left‑ventricular dysfunction because it can provoke ventricular arrhythmias.
Propafenone
Propafenone is another classIC agent with mild beta‑blocking properties. Doses range from 150‑300mg twice daily for maintenance or 600mg as a single‑dose conversion. Like flecainide, it’s contraindicated in structural heart disease.
Metoprolol (beta‑blocker only)
Metoprolol is a selective beta‑1 blocker. While it doesn’t address QT prolongation, it reduces heart rate and sympathetic triggers for atrial fibrillation. Doses start at 25‑50mg twice daily and may be increased to 200mg twice daily. It’s safe for most patients but offers less rhythm‑control than the classIII agents.

Side‑by‑Side Comparison
| Drug | Class | Primary Mechanism | Typical Dose | Major Side Effects | Monitoring Needs |
|---|---|---|---|---|---|
| Betapace (Sotalol) | III + β‑blocker | K⁺ channel blockade + β‑adrenergic blockade | 80‑160mg BID | QT prolongation, fatigue, bronchospasm | QTc daily x 7days, renal function |
| Amiodarone | III (multichannel) | Blocks Na⁺, K⁺, Ca²⁺, β‑receptors | 800‑1200mg loading, then 100‑200mg daily | Thyroid, pulmonary, hepatic toxicity | TSH, LFTs, chest X‑ray every 6months |
| Dofetilide | III | K⁺ channel blockade | 500µg BID (CrCl‑adjusted) | QT prolongation, torsades | In‑hospital ECG 4days, renal clearance |
| Flecainide | IC | Fast Na⁺ channel block | 200‑300mg single dose (conversion) | Pro‑arrhythmia in structural heart disease | Baseline ECG, avoid in CAD/LV dysfunction |
| Propafenone | IC | Na⁺ block + mild β‑blockade | 150‑300mg BID (maintenance) / 600mg single | Bradycardia, dizziness | ECG, avoid in CAD/LV dysfunction |
| Metoprolol | β‑blocker | Selective β‑1 antagonism | 25‑50mg BID up to 200mg BID | Bronchospasm, fatigue | Heart rate, blood pressure |
Choosing the Right Drug for You
Think of anti‑arrhythmic selection as a matchmaking process. Start with your underlying heart condition, then weigh each drug’s strengths against its drawbacks.
- Is your rhythm problem atrial fibrillation or ventricular tachycardia? Betapace and amiodarone cover both; flecainide and propafenone focus on atrial fibrillation.
- Do you have structural heart disease? Avoid classIC agents (flecainide, propafenone) and consider Betapace, amiodarone, or dofetilide, which are safer in that setting.
- What’s your kidney function? Sotalol and dofetilide require dose cuts when creatinine clearance falls below 50mL/min.
- Can you handle intensive monitoring? If frequent ECG checks or hospital stays are a barrier, metoprolol or low‑dose sotalol may be more practical.
- Are long‑term organ toxicities a concern? Amiodarone’s multi‑organ side‑effect profile makes it a last‑resort option despite its potency.
Discuss these points with your cardiologist; they can run labs, calculate renal dosing, and set up the necessary monitoring plan.
Practical Tips for Safe Use
- Always have a baseline ECG before starting any classIII drug.
- Check electrolytes (K⁺, Mg²⁺) - low levels heighten QT risk.
- Notify your provider of any new antibiotics, antifungals, or anti‑psychotics, as they often prolong QT.
- Use a medication card that lists dose, timing, and red‑flag symptoms (palpitations, dizziness, fainting).
- Schedule follow‑up labs within the first week for sotalol, and every 3‑6months for amiodarone.
Frequently Asked Questions
Can I switch from Betapace to Amiodarone without a wash‑out period?
Both drugs affect the QT interval, so a short wash‑out (usually 48hours) is recommended to avoid additive prolongation. Your doctor will tailor the timing based on your ECG results.
Is Betapace safe during pregnancy?
Sotalol crosses the placenta and can cause fetal arrhythmias. It’s generally avoided unless the benefits clearly outweigh the risks, and close fetal monitoring is required.
What should I do if I feel faint after taking Betapace?
Fainting may signal excessive heart‑rate slowing or a QT‑related event. Sit or lie down, call your clinic immediately, and have an ECG performed as soon as possible.
Can I take over‑the‑counter antihistamines with Betapace?
Many antihistamines are safe, but some (e.g., diphenhydramine) can modestly prolong QT. Review any new OTC drug with your pharmacist before use.
How long does it take for Betapace to reach steady‑state?
Sotalol’s half‑life is about 12hours, so steady‑state is typically reached after 3‑4days of twice‑daily dosing, assuming normal kidney function.
Rod Maine
September 30, 2025 AT 13:22Well, if you’re actually interested in the electrophysiological nuances of sotalol, you’d appreciate that it isn’t just a "beta‑blocker with a side‑effect". It uniquely merges class III potassium channel blockade with β‑adrenergic antagonism, which most textbooks gloss over. But the real kicker is the QT‑prolongation risk-something you can’t ignore even if you love fancy drug combos. The guide does a decent job, though it could've dived deeper into the pharmacogenomic variances. Still, a solid starter for anyone dabbling in anti‑arrhythmics.
Othilie Kaestner
October 1, 2025 AT 16:22Honestly, most of this guide is just hype; the real world uses amiodarone almost exclusively.
Sebastian Samuel
October 2, 2025 AT 19:22Okay, let’s cut the BS – sotalol can be a lifesaver, but only if you actually follow the QT monitoring schedule 🩺. Skipping those checks is a recipe for torsades, and nobody wants that nightmare 😱. The guide’s checklist is handy, but you still need a clinic that can do daily ECGs for a week. If your hospital can’t commit, you’re better off with a safer beta‑blocker. Bottom line: use it responsibly or don’t use it at all.
Mitchell Awisus
October 3, 2025 AT 22:22That’s a fair point; the monitoring burden is often under‑estimated, especially in outpatient settings. Moreover, renal function plays a huge role – any drop in creatinine clearance mandates dose reduction, which many clinicians overlook. It’s also worth noting that sotalol’s half‑life means steady‑state isn’t reached until about four days, so early ECGs might not reflect the final QT effect. In practice, pairing the drug with electrolyte management (keeping K⁺ > 4 mmol/L) can mitigate some risks. All in all, the guide’s emphasis on labs and ECGs is spot‑on, but real‑world logistics can be tricky.
Annette Smith
October 5, 2025 AT 01:22Choosing the right rhythm drug is like choosing a path in life; you must weigh benefit against risk, and accept the consequences of your choice. Simplicity often wins – if you can’t commit to monitoring, a safer option may bring peace of mind.
Joy Arnaiz
October 6, 2025 AT 04:22One must approach the prescription of Betapace with the utmost caution, for hidden conspiracies within pharmaceutical lobbying may obscure subtle dangers that only the vigilant can perceive.
Christopher Eyer
October 7, 2025 AT 07:22While the guide presents a seemingly balanced overview of sotalol and its alternatives, it fails to address the systemic bias that pervades modern cardiology. First, the emphasis on “monitoring capacity” subtly pushes patients toward hospital‑based care, which benefits large health systems financially. Second, the claim that amiodarone is a “last‑resort” ignores decades of evidence showing its superior mortality benefit in certain sub‑populations. Third, the discussion of renal dosing is oversimplified; creatinine clearance calculations vary widely across labs, leading to dangerous dosing errors. Fourth, the guide does not mention the prevalence of off‑label sotalol use in patients with mild structural disease, a practice that many cardiologists quietly endorse. Fifth, the side‑effect profile of sotalol is presented as manageable, yet real‑world data indicate a higher incidence of torsades than reported in trials. Sixth, the recommendation to avoid flecainide in any structural heart disease is too absolute; recent studies suggest selective use may be safe under strict imaging guidance. Seventh, the lack of mention of drug‑drug interactions with contemporary anti‑psychotics is a glaring omission, considering the rising polypharmacy trend. Eighth, the guide assumes patients have ready access to daily ECGs, which is unrealistic in many rural settings. Ninth, the discussion of beta‑blockers like metoprolol fails to acknowledge their role in heart failure with reduced ejection fraction, an area where sotalol is contraindicated. Tenth, the article’s tone subtly discourages patient autonomy by emphasizing physician‑driven decision making. Eleventh, the table’s formatting is ambiguous, potentially leading to misinterpretation of dosing ranges. Twelfth, the guide does not address the cost disparities between generic sotalol and brand‑name amiodarone, which can influence prescribing patterns. Thirteenth, there is no mention of ongoing clinical trials that may soon shift the paradigm away from class III agents altogether. Fourteenth, the brief mention of electrolyte monitoring overlooks magnesium’s critical role in stabilizing the myocardium. Finally, the overall narrative appears to serve as a marketing tool for sotalol rather than an unbiased clinical resource, and such bias must be critically examined.
Mike Rosenstein
October 8, 2025 AT 10:22Christopher, you raise several valid concerns, particularly regarding accessibility of monitoring and the subtle financial incentives. However, it’s also important to recognize that the guide does aim to provide a practical decision‑making framework for clinicians who must balance efficacy, safety, and resource constraints. While some nuances could be expanded, the core recommendations align with current guideline consensus. A collaborative approach, incorporating patient preferences and local capabilities, can mitigate many of the systemic issues you highlighted.
Ada Xie
October 9, 2025 AT 13:22It is imperative that any comparative analysis of anti‑arrhythmic agents adhere strictly to precise terminology, avoid colloquialism, and maintain consistent use of the International System of Units throughout.
Brian Koehler
October 10, 2025 AT 16:22Indeed, Ada! Precision is the backbone of effective medical communication; yet we must also remember to infuse a dash of creativity to keep readers engaged-think of it as a well‑crafted symphony where each term plays its part in harmony.
Vishnu Raghunath
October 11, 2025 AT 19:22So they tell us to trust the “guidelines” while the real story is buried under layers of bureaucracy and profit‑driven motives.
Aparna Dheep
October 12, 2025 AT 22:22Honestly the whole anti‑arrhythmic debate feels like a circus where everyone argues about the same tired tricks.
Sangeeta Birdi
October 14, 2025 AT 01:22It’s easy to feel overwhelmed by the jargon and conflicting opinions, but remembering that each patient’s experience is unique can guide us toward more compassionate choices 😊.