Bystolic (Nebivolol) vs. Other Hypertension Drugs: Complete Comparison
 Oct, 1 2025
Oct, 1 2025
Bystolic (Nebivolol) vs. Other Hypertension Drugs Comparison Tool
Comparison Results
When doctors prescribe a pill for high blood pressure, the name on the bottle can feel like a cryptic code. Bystolic (nebivolol) is one of those codes, but how does it really stand up against the other options in the hypertension toolbox? This guide breaks down nebivolol’s mechanism, its pros and cons, and puts it side‑by‑side with the most common alternatives so you can see which drug fits your health goals.
- Nebivolol is a third‑generation beta blocker that also releases nitric oxide, helping vessels relax.
- It’s especially good for patients who need both lower heart rate and better vascular tone.
- Common alternatives include older beta blockers (atenolol, metoprolol), ACE inhibitors (lisinopril), ARBs (losartan) and calcium‑channel blockers (amlodipine).
- Each class has distinct side‑effect profiles and suitability for conditions like diabetes, asthma, or kidney disease.
- Choosing the right drug is a balance of efficacy, tolerability, cost and personal health factors.
What Is Bystolic (Nebivolol)?
Nebivolol is a third‑generation beta‑adrenergic blocker that uniquely promotes nitric oxide release, leading to vasodilation while still slowing the heart. Marketed as Bystolic, it was approved by the FDA in 2007 for managing hypertension.
Key attributes:
- Selective for β1 receptors (cardiac) with minimal β2 effect (lung), reducing risk of bronchospasm.
- Enhances endothelial nitric oxide synthase, improving arterial compliance.
- Available in 2.5mg, 5mg, and 10mg tablets; once‑daily dosing.
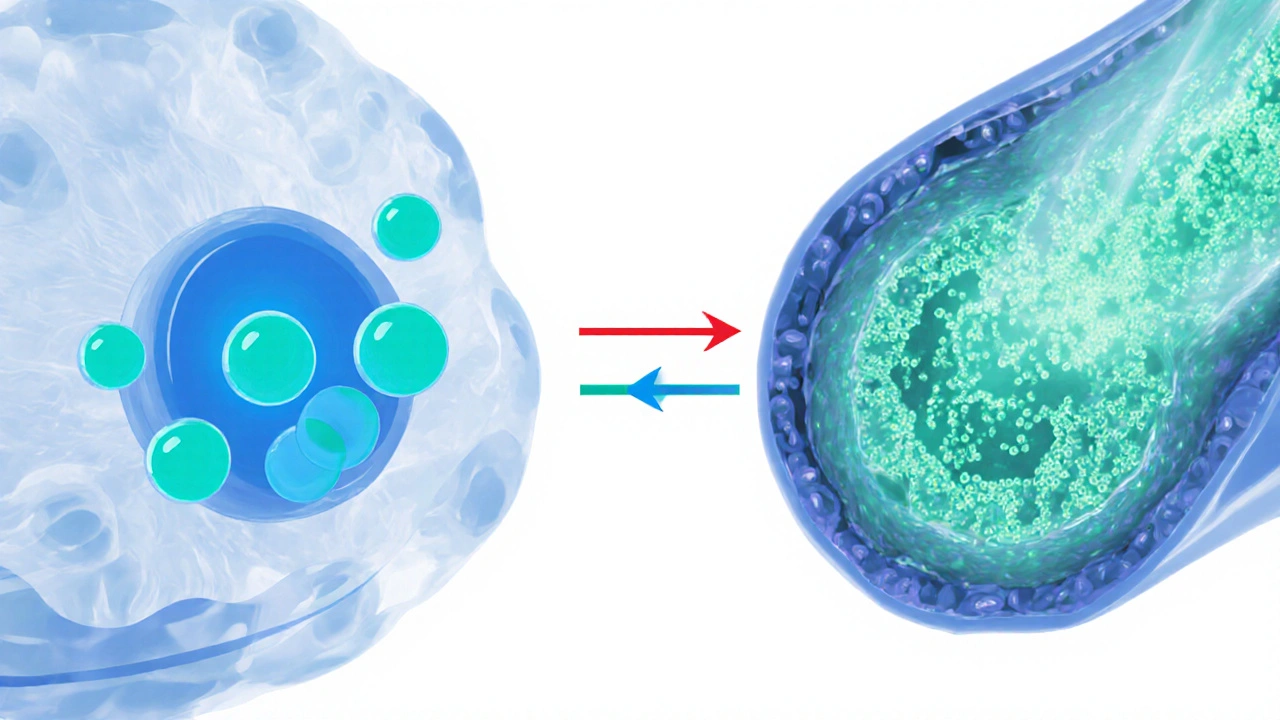
How Nebivolol Lowers Blood Pressure
The drug works on two fronts. First, its beta‑blocking action reduces heart rate and contractility, cutting cardiac output. Second, the nitric‑oxide pathway relaxes smooth muscle in the arterial wall, lowering systemic vascular resistance. This dual action often yields a more pronounced drop in systolic pressure compared with older beta blockers.
Clinical studies from 2019‑2023 show an average reduction of 10‑12mmHg systolic and 5‑7mmHg diastolic after eight weeks of therapy at a 5mg dose, with a heart‑rate reduction of about 8 beats per minute.
Pros and Cons of Bystolic
Every medication has trade‑offs. Here’s a quick snapshot.
| Aspect | Advantage | Disadvantage |
|---|---|---|
| Mechanism | β1‑selective + nitric‑oxide mediated vasodilation | Complex pharmacology may cause variable response |
| Heart Rate | Gentle reduction, beneficial for tachycardia | May be too low for athletes needing higher HR |
| Metabolic Effects | Neutral on glucose; safe for diabetics | Rare cases of mild fatigue |
| Drug Interactions | Fewer than older β‑blockers | Interactions with CYP2D6 inhibitors (e.g., fluoxetine) |
| Side‑Effect Profile | Lower incidence of bronchospasm, erectile dysfunction | Occasional dizziness on standing |
How Bystolic Stacks Up Against Other Beta Blockers
Older beta blockers like atenolol and metoprolol are still widely prescribed, largely because they’re cheap and well‑known. Yet they lack nebivolol’s nitric‑oxide boost.
| Drug | β‑Selectivity | Vasodilatory Action | Typical Dose | Key Side Effects |
|---|---|---|---|---|
| Nebivolol | High (β1‑selective) | Yes - nitric‑oxide mediated | 2.5‑10mg daily | Dizziness, mild fatigue |
| Atenolol | Moderate | No | 25‑100mg daily | Cold extremities, erectile dysfunction |
| Metoprolol | High | No | 50‑200mg daily | Bradycardia, fatigue |
If you have asthma or severe chronic obstructive pulmonary disease (COPD), nebivolol’s β2‑spareness often makes it a safer bet than atenolol, which can trigger bronchoconstriction.
Comparing Bystolic to ACE Inhibitors and ARBs
ACE inhibitors (e.g., lisinopril) and angiotensinII receptor blockers (ARBs, e.g., losartan) act upstream of the beta‑adrenergic system by relaxing vessels through the renin‑angiotensin‑aldosterone pathway.
| Class | Primary Target | Typical Dose Range | Pros | Cons |
|---|---|---|---|---|
| ACE Inhibitor (Lisinopril) | ACE enzyme | 5‑40mg daily | Renoprotective, good for diabetics | Cough, hyperkalemia |
| ARB (Losartan) | AT1 receptor | 25‑100mg daily | Less cough, protects kidneys | Potential for dizziness |
| Bystolic (Nebivolol) | β1‑receptor + nitric‑oxide | 2.5‑10mg daily | Low heart‑rate impact, metabolically neutral | Higher cost, CYP2D6 interaction |
Patients with chronic kidney disease often benefit more from ACE inhibitors or ARBs because of their proven renoprotective effect. Nebivolol doesn’t directly protect the kidneys, but its neutral effect on glucose makes it a solid secondary choice when an ACE inhibitor isn’t tolerated.
Calcium‑Channel Blockers (CCBs) in the Mix
CCBs such as amlodipine widen arteries by blocking calcium entry into smooth muscle cells. They’re great for isolated systolic hypertension, especially in older adults.
| Drug | Mechanism | Blood‑Pressure Effect | Typical Dose | Common Side Effects |
|---|---|---|---|---|
| Bystolic | β1‑block + NO vasodilation | 10‑12mmHg systolic | 2.5‑10mg daily | Dizziness, fatigue |
| Amlodipine | L-type calcium‑channel blockade | 12‑15mmHg systolic | 2.5‑10mg daily | Peripheral edema, flushing |
If you’re prone to swelling in your ankles, nebivolol avoids that CCB drawback. However, amlodipine can be more effective for isolated systolic spikes that often appear after age 60.
Decision Guide: When to Pick Bystolic
Below is a quick decision tree you can run through with your clinician.
- Do you have asthma or COPD? - If yes, choose nebivolol over non‑selective beta blockers.
- Is diabetes a concern? - Nebivolol’s neutral impact on glucose makes it preferable to thiazide diuretics.
- Is renal protection a priority? - ACE inhibitors or ARBs win here.
- Do you experience frequent ankle swelling? - Skip CCBs like amlodipine; consider nebivolol.
- Are you on a tight budget? - Generic atenolol or metoprolol may be cheaper, but weigh side‑effect risk.
In short, nebivolol shines for patients who need heart‑rate control, have mild to moderate hypertension, and want a low‑risk metabolic profile.
Practical Tips for Starting Nebivolol
- Take the pill at the same time each day, preferably in the morning.
- Monitor your blood pressure and heart rate for the first two weeks; a drop of 5‑10bpm is expected.
- Watch for dizziness when you stand up - rise slowly to avoid falls.
- If you’re on a CYP2D6 inhibitor (like fluoxetine), ask your doctor about dose adjustment.
- Ask about generic nebivolol options; they can cut cost by up to 30%.
Frequently Asked Questions
Can nebivolol be used during pregnancy?
Nebivolol is classified as Category C, meaning risk cannot be ruled out. Most clinicians prefer safer options like labetalol or methyldopa during pregnancy.
How quickly does Bystolic start working?
Blood‑pressure lowering effects can be seen within 2‑4hours, but the full steady‑state impact usually takes about 2weeks.
Is nebivolol safe for people with heart failure?
Yes, nebivolol is approved for chronic heart failure (NYHA class II‑III). It improves ejection fraction and reduces hospitalization rates compared with placebo.
What should I do if I miss a dose?
Take the missed tablet as soon as you remember, unless it’s almost time for the next dose. In that case, skip the missed one and continue with your regular schedule. Never double‑dose.
Can Bystolic be combined with other hypertension drugs?
Combining nebivolol with an ACE inhibitor, ARB, or low‑dose diuretic is common practice and often yields better control without adding major side effects.
Bottom line: nebivolol offers a unique blend of beta‑blocking and vasodilating actions that can make it a better fit for certain patients than classic beta blockers, ACE inhibitors, ARBs or CCBs. Talk with your healthcare provider about your full medical picture, and use this comparison to ask the right questions.
Ira Andani Agustianingrum
October 1, 2025 AT 22:08Hey folks, if you’re trying to decide whether Bystolic is right for you, think of it like a two‑in‑one tool – it calms the heart *and* relaxes the vessels. The β1‑selectivity means lungs stay clear, which is a big win for anyone with a sniffly airway. Because it also releases nitric oxide, you often see a smoother drop in systolic numbers without the usual “cold hands” feeling. I’ve seen patients on it bounce back to their morning jogs faster than on older beta‑blockers. Just keep an eye on that first‑week dizziness and you’ll be golden.
James Higdon
October 2, 2025 AT 12:13It is incumbent upon the medical community to scrutinize the economic barriers that accompany novel antihypertensive agents such as nebivolol. While the pharmacologic profile appears advantageous, the elevated price point may exacerbate health inequities among underserved populations. Physicians bear a moral responsibility to weigh cost‑effectiveness alongside clinical efficacy. Informed consent must therefore include a transparent discussion of financial implications.
Wanda Smith
October 3, 2025 AT 02:06One might contemplate the hidden architectures that dictate which drugs rise to prominence on pharmacy shelves. Nebivolol, with its dual β‑blockade and nitric‑oxide release, is presented as a marvel of modern science, yet the very same patents are often held by conglomerates that profit from obscurity. Is the emphasis on “vascular relaxation” a subtle narrative to steer clinicians away from older, cheaper generics? The silent chorus of regulatory agencies, funded in part by those same corporations, rarely questions the pricing schema. Moreover, the whispered warnings about “CYP2D6 inhibitors” may serve as a gatekeeper, ensuring that only patients who can afford specialized monitoring receive the drug. When we peel back the layers, we encounter a pattern: innovation touted as progress, while accessibility is quietly eroded. The patient, therefore, becomes a pawn in a grander economic chess game, unaware of the silent moves. In the end, the true measure of a medication is not only its millimetric blood‑pressure reduction but also its role in sustaining or dismantling systemic inequities.
Bridget Jonesberg
October 3, 2025 AT 16:00Within the pantheon of antihypertensive pharmacotherapy, nebivolol occupies a niche that is as academically intriguing as it is clinically significant. Its mechanistic elegance, marrying β1‑selectivity with endothelium‑derived nitric oxide, distinguishes it from the pedestrian profiles of atenolol or metoprolol. Yet one must acknowledge that the empirical data, while robust, are not universally translatable across diverse ethnic cohorts. The discourse surrounding its cost‑effectiveness, therefore, warrants a more nuanced, perhaps even aristocratic, deliberation. In practice, a clinician’s choice should reflect both biochemical sophistication and pragmatic patient‑centred considerations.
Marvin Powers
October 4, 2025 AT 05:53Alright, let’s unpack nebivolol with the fervor of a hype‑train at full throttle. First off, the drug isn’t just another beta‑blocker; it’s a third‑generation marvel that throws nitric oxide into the mix, which means you’re getting vasodilation on top of heart‑rate control. That double‑hit translates to a more noticeable dip in systolic pressure – think 10 to 12 mmHg, which is nothing to sneeze at when you’re battling stage‑2 hypertension. Because it’s β1‑selective, the lungs get a pass; patients with mild asthma can breathe easier compared to the old‑school non‑selective crew. The side‑effect profile is relatively tame: a bit of dizziness here, some fatigue there, but you’re less likely to see the dreaded cold extremities or erectile dysfunction that haunt atenolol users. Now, cost. Yes, nebivolol carries a premium, but the price tag can be softened by hunting down generic versions or patient‑assistance programs – a tip that many forget to mention in the glossy brochures. When you pair it with an ACE inhibitor or low‑dose diuretic, the synergy often means you can keep doses low and side‑effects lower, a win‑win for adherence. The drug’s neutral effect on glucose is a particular boon for diabetic patients, who often get catapulted onto thiazides that mess with sugar control. From a practical standpoint, you want to start at 5 mg once daily and titrate based on response – most clinicians see a heart‑rate drop of about 8 bpm within the first two weeks. Keep an eye on orthostatic dizziness; rising slowly from a chair can spare you a fall. And if you happen to be on a CYP2D6 inhibitor like fluoxetine, a dose reduction isn’t just a nice idea, it’s a necessity. In terms of long‑term outcomes, studies from 2019‑2023 show nebivolol reduces hospitalizations for heart failure more effectively than many older β‑blockers, a fact that should make cardiologists sit up straight. But remember, it’s not a miracle cure – lifestyle changes still rule the roost. Exercise, sodium reduction, and weight control remain the backbone of any hypertension regimen. So, if you fit the profile – mild‑to‑moderate hypertension, maybe a hint of tachycardia, occasional asthma, and you can swing the cost – nebivolol is a solid contender worth a serious look.
Christopher Montenegro
October 4, 2025 AT 19:46The assertion that nebivolol's price alone dictates inequity overlooks the pharmacoeconomic models that quantify quality‑adjusted life years. A cost‑effectiveness ratio below $50,000/QALY is widely accepted, and nebivolol frequently meets that threshold when used in heart‑failure cohorts. Thus, the moral indictment is misplaced without granular budget impact analyses.
Kyle Olsen
October 5, 2025 AT 09:40Really? The “hidden architectures” narrative sounds like a bedtime story for the conspiracy‑crazed. The data are out there, peer‑reviewed, and not some clandestine plot. Stick to the facts.
Sarah Kherbouche
October 5, 2025 AT 23:33i cant beleive how u talk abt nebivolol like its some elite club secret. it's just a pill that works, no need for all that fancy talk. get on with it.
MANAS MISHRA
October 6, 2025 AT 13:26Thanks for the thorough breakdown! You’ve highlighted the key points without drowning us in jargon, and the practical tips about dose titration and cost‑saving options are especially helpful. I’ll definitely bring these up with my doctor.
Lawrence Bergfeld
October 7, 2025 AT 03:20Cost can be a deal‑breaker.
Jai Patel
October 7, 2025 AT 17:13Absolutely! While a pricey tag can sting, remember that the health payoff might just outweigh the wallet hit – especially when you’re dodging hospital readmissions.
Zara @WSLab
October 8, 2025 AT 07:06🤔 Curious, anyone know if insurance usually covers the generic version? 🤷♀️
Randy Pierson
October 8, 2025 AT 21:00The comparative tables in the article do a solid job of laying out mechanisms, but a visual chart would make the differences pop even more for quick reference.
Bruce T
October 9, 2025 AT 10:53True, a graphic could bridge the gap between clinicians and patients who aren’t fluent in medical lingo. Simplicity wins.
Darla Sudheer
October 10, 2025 AT 00:46Nice summary of the pros and cons.
Elizabeth González
October 10, 2025 AT 14:40While the enumeration of benefits and drawbacks is concise, it invites reflection on the broader ethical dimensions of prescribing practices, particularly regarding accessibility and informed consent.
Joy Arnaiz
October 11, 2025 AT 04:33One must also consider how pharmaceutical lobbying subtly shapes those very prescribing norms, steering clinicians toward higher‑margin drugs under the guise of “innovation.”