Children and Antihistamines: Safe Dosing by Age and What Parents Must Know
 Nov, 10 2025
Nov, 10 2025
Children's Antihistamine Dosing Calculator
Medication Selection
Important Safety Information
When your child breaks out in hives after eating peanuts, or their eyes water and nose runs every spring, it’s tempting to reach for the old bottle of Benadryl. But giving antihistamines to kids isn’t like giving them fever medicine. The wrong dose, the wrong type, or even the wrong timing can lead to serious side effects - or worse. Today, pediatric guidelines have changed dramatically. What was once common practice is now considered risky. And if you’re unsure what to give your child, you’re not alone. Many parents are still using outdated advice.
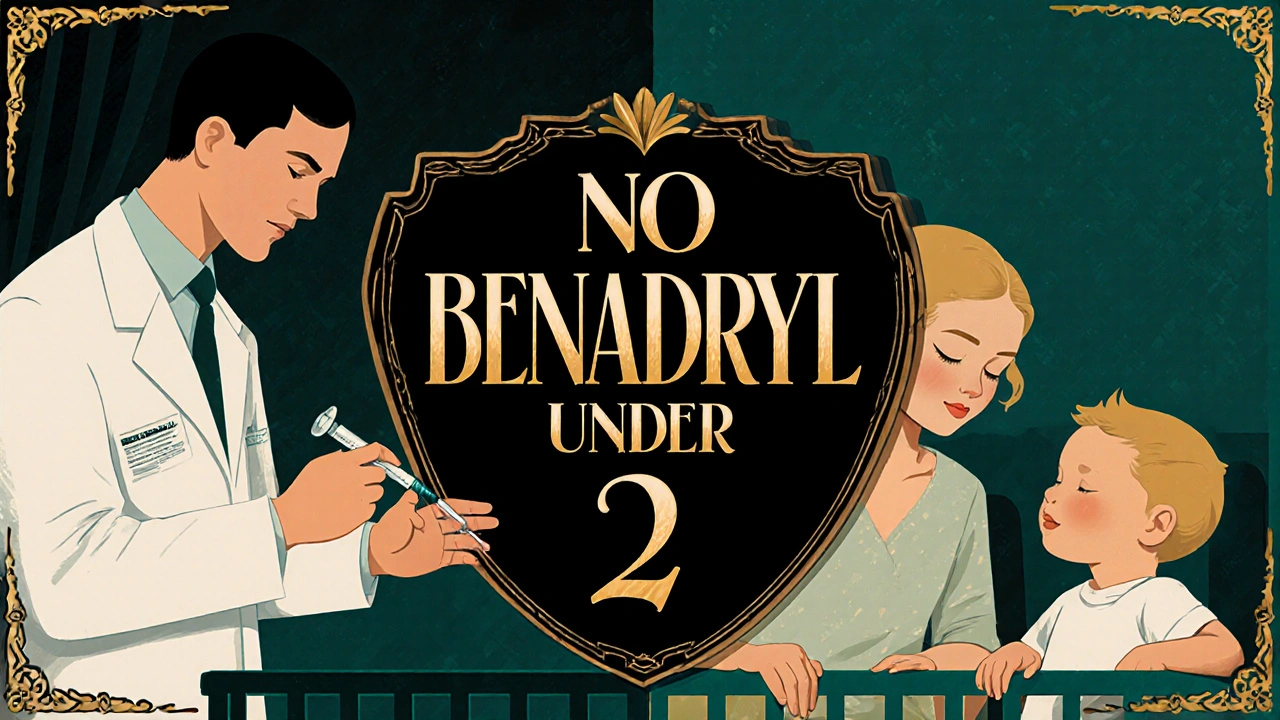
Why First-Generation Antihistamines Like Benadryl Are Risky for Kids
Diphenhydramine, the active ingredient in Benadryl, has been around for decades. It works fast - often relieving symptoms in 15 to 30 minutes. But that speed comes at a cost. This type of antihistamine crosses the blood-brain barrier easily, which means it doesn’t just block allergy signals - it slows down the brain.
In children, especially under age 2, this can cause extreme drowsiness, confusion, dry mouth, rapid heartbeat, or even seizures. A 2020 study in the Journal of Pediatric Allergy and Immunology found that 50 to 60% of young children given diphenhydramine became noticeably sleepy. Some became agitated instead, a paradoxical reaction that can look like hyperactivity or temper tantrums. These effects aren’t just inconvenient - they’re dangerous.
The FDA has warned since 2008 that diphenhydramine should not be used in children under 2 without a doctor’s supervision. Even for older kids, giving it for sleep - a common habit among parents - increases overdose risk by 300%. The American Academy of Pediatrics says this practice is not only ineffective for sleep but actively harmful.
Second-Generation Antihistamines Are the New Standard
Thankfully, safer options exist. Cetirizine (Zyrtec) and loratadine (Claritin) are second-generation antihistamines. They don’t cross the blood-brain barrier as easily, so they cause far less drowsiness and have fewer side effects. Studies show only 10 to 15% of children on cetirizine feel sleepy - compared to 6.9% on loratadine. That’s why hospitals like Boston Children’s, Children’s Hospital Colorado, and St. Louis Children’s now recommend these as the first choice for most childhood allergies.
They also last longer. While Benadryl wears off in 4 to 6 hours and needs to be given every 4 to 6 hours, cetirizine and loratadine work for 24 hours. That means one dose a day - fewer chances for dosing errors, fewer disruptions to sleep or school, and less stress for families.
Exact Dosing Guidelines by Age and Weight
Dosing isn’t just about age. It’s about weight. And using a kitchen spoon? That’s a recipe for error. Studies show kitchen teaspoons vary by 20 to 50% in volume. Always use the measuring cup or syringe that comes with the medicine.
- Babies 6 to 11 months: Cetirizine at 0.125 mg per kg of body weight per day. For an 8 kg (18 lb) baby, that’s about 1 mg daily. If symptoms persist after a few days, a doctor may increase it to 0.25 mg/kg/day. This is off-label use, but supported by clinical evidence and recommended by experts like Dr. Eric Macy of the AAAAI.
- Children 1 to 2 years: Cetirizine 2.5 mg once daily (½ teaspoon of 5 mg/5 mL liquid). Loratadine is not FDA-approved for this age group, so cetirizine is preferred.
- Children 2 to 5 years: Cetirizine or loratadine, 5 mg once daily. That’s one teaspoon of liquid (5 mg/5 mL) or one children’s chewable tablet (check the label - some are 5 mg, others are 10 mg).
- Children 6 to 11 years: Cetirizine 5 to 10 mg daily (1 to 2 teaspoons liquid or one 5 mg chewable, sometimes two). Loratadine 5 mg daily (1 teaspoon liquid or one tablet).
- Children 12 and older: 10 mg daily of either cetirizine or loratadine - same as adult dose.
For diphenhydramine, if prescribed by a doctor for an acute reaction: children weighing 38 to 49 pounds get 7.5 mL of liquid (12.5 mg) every 6 hours, no more than 6 doses in 24 hours. Never give it without clear instructions.
What to Avoid at All Costs
Many over-the-counter allergy products contain more than one active ingredient. Decongestants like pseudoephedrine or phenylephrine are sometimes added to antihistamines. These are not recommended for children under 6. They can raise blood pressure, cause heart palpitations, and lead to dangerous overdoses.
Another common mistake: using adult tablets for kids. A 10 mg loratadine tablet is not a “half-dose” for a 5-year-old. Cutting pills is unreliable and risky. Always use the pediatric formulation.
And never use antihistamines to make a child sleepy. Even if it works, it’s not safe. The American College of Allergy, Asthma, and Immunology says this practice is linked to a threefold increase in accidental overdoses in children under 2.
When to Call a Doctor or Poison Control
Most allergic reactions in kids are mild - hives, runny nose, itchy eyes. But if your child develops swelling of the lips or tongue, trouble breathing, vomiting, or fainting, that’s an emergency. Call 911 or go to the ER. Antihistamines won’t stop anaphylaxis. Epinephrine is the only treatment.
If you suspect an overdose - even if your child seems fine - call Poison Control immediately at 1-800-222-1222. Signs include:
- Extreme drowsiness or unresponsiveness
- Fast or irregular heartbeat
- Dilated pupils or blurry vision
- Confusion, hallucinations, or agitation
- Difficulty urinating or dry, flushed skin
These symptoms can develop quickly. Don’t wait. Even small overdoses in young children can be life-threatening.
What’s Changing in 2025 and Beyond
Research is moving fast. In 2024, the FDA required new safety studies for all antihistamines used in children under 2. Results are expected by late 2025. Early data from ongoing trials (NCT04567821) suggest cetirizine may soon be approved for infants under 6 months - something currently done off-label under specialist care.
Meanwhile, pediatric allergists are seeing a shift in practice. Since 2018, prescriptions for second-generation antihistamines in children have risen by 17.3% each year. A 2023 survey by the AAAAI found that 94.7% of pediatric allergy specialists now recommend cetirizine or loratadine as first-line treatment. The days of Benadryl as a go-to for every sneeze are over.
But awareness hasn’t caught up. A CDC study found that nearly 30% of antihistamine use in children under 2 is off-label - and over 60% of those cases involve diphenhydramine. Many parents still think it’s the safest or fastest option. It’s not. The science is clear: newer is better.
Final Advice: Keep It Simple, Keep It Safe
If your child has mild allergies, start with cetirizine or loratadine. Use the correct dose based on weight. Use the measuring tool that comes with the medicine. Never use adult pills. Avoid anything with a decongestant. And never use antihistamines as sleep aids.
If you’re unsure - if your child is under 2, if symptoms are severe, or if you’ve given the wrong dose - call your pediatrician. There’s no shame in asking. Allergies are common. Getting the treatment right? That’s what keeps kids safe.
Can I give my 1-year-old Benadryl for allergies?
No - not without a doctor’s order. The FDA advises against using diphenhydramine (Benadryl) in children under 2 years due to risks of severe drowsiness, breathing problems, and seizures. For a 1-year-old with allergies, cetirizine (Zyrtec) at 2.5 mg daily is the safer, recommended option. Always check with your pediatrician first.
Is cetirizine safe for babies under 6 months?
Cetirizine is not yet FDA-approved for babies under 6 months, but experts like Dr. Eric Macy recommend it off-label in severe cases - such as persistent hives - at a starting dose of 0.125 mg per kg of body weight per day. This should only be done under the supervision of a pediatric allergist. Never give it without medical guidance.
How do I know if I’m giving the right dose?
Always use the measuring device that comes with the medicine - never a kitchen spoon. Check the label for mg per mL or per tablet. For example, children’s Zyrtec liquid is 5 mg per 5 mL. A 10 kg child would get 1.25 mL (0.125 mg/kg) if under 6 months, or 2.5 mL (0.25 mg/kg) if 6-11 months. If you’re unsure, ask your pharmacist or doctor to show you how to measure it.
Can I give my child Claritin and Zyrtec together?
No - don’t combine them. Both are antihistamines and work similarly. Taking both increases the risk of side effects without added benefit. Pick one and stick with it. If one doesn’t work after a week, talk to your doctor about switching or adjusting the dose - don’t double up.
Are chewable tablets safer than liquid for kids?
It depends on the dose. Some children’s chewables are 5 mg, others are 10 mg. If you give a 10 mg tablet to a 3-year-old who needs only 5 mg, you’ve doubled the dose. Always read the label. Liquid is easier to adjust for small weights, but chewables are fine if you know the exact mg per tablet and your child can safely chew and swallow them.
What should I do if my child accidentally takes too much?
Call Poison Control immediately at 1-800-222-1222 - even if your child seems fine. Symptoms like drowsiness, fast heartbeat, or confusion can appear hours later. Don’t wait. Keep the medicine bottle handy when you call so you can tell them exactly what was taken and how much.
Charity Peters
November 12, 2025 AT 18:02Used to give Benadryl to my toddler for sneezes. Learned the hard way when she got super hyper and then crashed for 12 hours. Never again. Zyrtec is way calmer for everyone.
Faye Woesthuis
November 13, 2025 AT 03:34If you're still using Benadryl on your kid, you're not just ignorant-you're dangerous. This post is basic pediatric safety 101. Stop winging it with kitchen spoons and Google advice.
raja gopal
November 14, 2025 AT 03:06As a dad from India, I was shocked to see how common Benadryl use is here too. We used to call it 'sleep medicine' for kids. Reading this made me check with my pediatrician-turned out my 3-year-old was on double the recommended dose. Thank you for this clear guide. Really saved us.
Samantha Stonebraker
November 14, 2025 AT 07:50There’s a quiet revolution happening in pediatric allergy care-and most parents don’t even know it. We’ve been clinging to Benadryl like a security blanket because it’s familiar, not because it’s safe. The real act of love isn’t reaching for the bottle-it’s pausing, reading the label, calling the doctor, and choosing the slower, smarter path. It’s messy. It’s inconvenient. But it’s the only path that keeps them truly safe.
Kevin Mustelier
November 15, 2025 AT 23:28Wow. So much info. Like, wow. 🤯 But honestly? If your kid has allergies, just give them a Zyrtec and move on. Why are we overcomplicating this? Also, why does everything have to be a 2000-word essay now? 😅
Keith Avery
November 17, 2025 AT 06:24Let’s be real-the AAP and FDA are just pushing pharma’s agenda. Cetirizine is just a branded version of diphenhydramine with a different molecular tweak. The ‘no brain effects’ claim is marketing spin. I’ve seen kids on Zyrtec act just as weird. This post is fearmongering dressed as science.
Luke Webster
November 19, 2025 AT 05:36Coming from a country where OTC meds are sold like candy, this post was a wake-up call. My cousin’s kid in Delhi was on Benadryl daily for ‘colds’-turns out it was seasonal allergies. After switching to loratadine, the tantrums stopped, the sleep improved, and the pediatrician actually smiled. Sometimes the simplest change is the most powerful one.
Natalie Sofer
November 19, 2025 AT 06:24Thank you for this. I just realized I’ve been giving my 4-year-old the wrong dose because I thought the chewable was 5mg but it was 10mg. 😳 I’m going to the pharmacy today to get the right stuff. Also, I can’t believe I used a teaspoon. So dumb. But now I know better.
Tiffany Fox
November 19, 2025 AT 14:21My kid had hives for weeks. Benadryl didn’t help. Zyrtec? Gone in 2 days. No drowsiness, no chaos. Just peace. Don’t overthink it-use the right tool for the job.
Rohini Paul
November 21, 2025 AT 01:40Wait, so we’re saying Benadryl is bad but Zyrtec is fine? But what if your kid hates the taste? I tried Zyrtec liquid and it was like giving them poison. Chewable? Too big. What then? No one talks about the practical stuff.
Courtney Mintenko
November 22, 2025 AT 05:02Benadryl is the reason my cousin’s kid ended up in the ER. I told her not to give it. She said ‘but it worked last time.’ Now she’s in therapy for guilt. This post should be mandatory. Parents need to stop pretending they know medicine.
Sean Goss
November 22, 2025 AT 21:49The entire premise is flawed. The cited 2020 study had a sample size of n=47. The FDA warning is based on case reports, not RCTs. You're conflating off-label use with contraindication. And why are you promoting cetirizine? It's a patent-protected, overpriced molecule with no superior efficacy data in children under 2. This is evidence-free alarmism disguised as clinical guidance.
Khamaile Shakeer
November 22, 2025 AT 22:25Okay, but what about the 2023 study from Mumbai where they gave diphenhydramine to 500 kids and only 3 had side effects? 🤔 Also, I give my kid Benadryl + Zyrtec together and he’s fine! 😎 Maybe the real problem is overdiagnosis of allergies? Just saying… 🤷♂️
Suryakant Godale
November 24, 2025 AT 00:14Respectfully, the clinical recommendations cited are consistent with current global pediatric allergology standards as outlined in the 2022 EAACI Guidelines and the 2023 AAAAI Position Statement on Pediatric Antihistamine Use. The weight-based dosing protocol for cetirizine in infants is supported by pharmacokinetic modeling and has been validated in multicenter observational cohorts. It is imperative that caregivers adhere to precise dosing instruments and avoid polypharmacy. This is not a matter of preference but of pharmacological safety.