Chronic Kidney Disease: Understand the Stages, How It Progresses, and Why Early Detection Saves Lives
 Jan, 12 2026
Jan, 12 2026
Most people don’t realize their kidneys are failing until it’s too late. That’s because chronic kidney disease (CKD) doesn’t scream for attention. No sharp pain. No fever. Just quiet, slow damage - often going unnoticed until 80% of kidney function is gone. By then, dialysis or a transplant may be the only options left. But here’s the truth: chronic kidney disease doesn’t have to reach that point. If caught early, progression can be slowed - even stopped - in many cases.
What Exactly Is Chronic Kidney Disease?
Chronic kidney disease isn’t a single illness. It’s a label for when your kidneys are damaged and can’t filter blood the way they should. This damage lasts at least three months. It’s not a sudden crash like a heart attack. It’s more like a leaky faucet you ignore until the floor is underwater. Your kidneys do more than just make urine. They balance fluids, remove toxins, control blood pressure, make red blood cell signals, and keep your bones strong. When they fail, everything else starts to unravel. The good news? The medical community has a clear, science-backed way to track this damage - and it’s called staging.The Six Stages of CKD: What Your eGFR Really Means
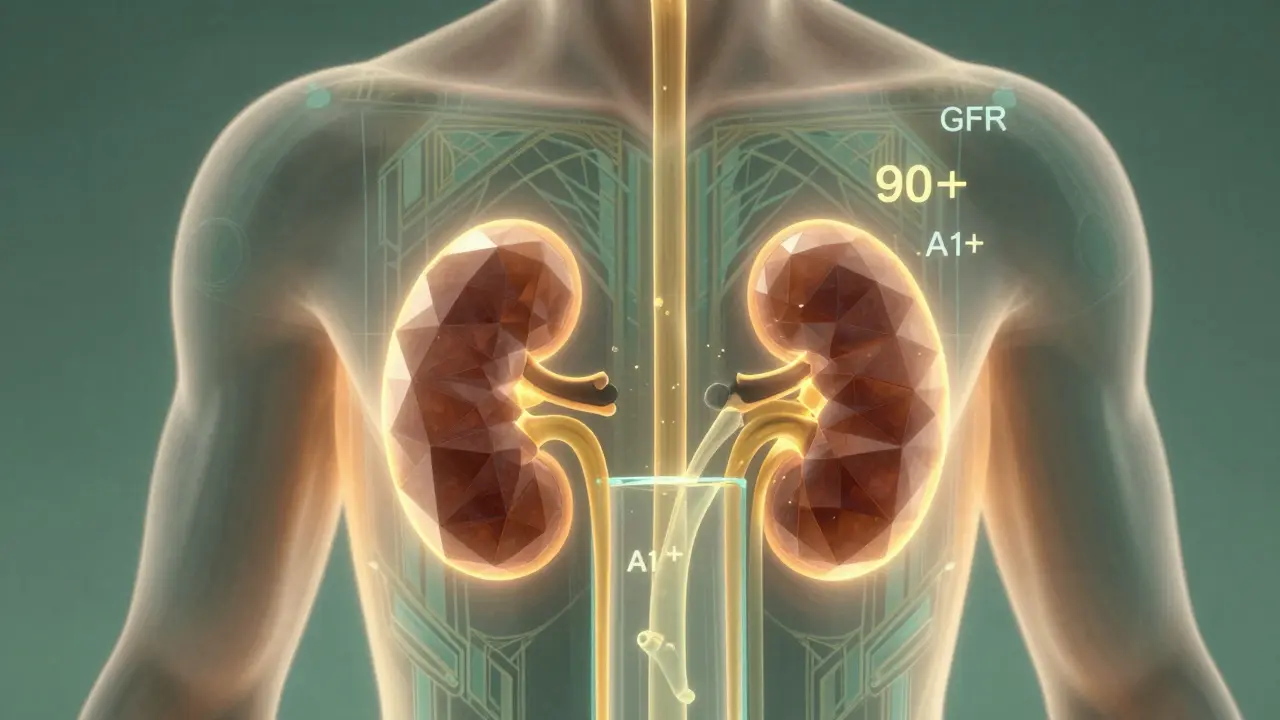
Doctors don’t guess how bad your kidney disease is. They measure it. The key number is eGFR - estimated glomerular filtration rate. It tells you how well your kidneys are filtering waste from your blood. The higher the number, the better the function. Normal is 90 or above. Here’s how the stages break down, based on the 2012 KDIGO guidelines still used today:- Stage G1: eGFR 90+ - Your kidneys look normal on paper, but there’s damage. This could mean protein in your urine, abnormal imaging, or scarring seen on biopsy. You might feel fine, but your kidneys are sending warning signals.
- Stage G2: eGFR 60-89 - Mild reduction. Kidney function is still mostly working, but damage is confirmed. Many people here are undiagnosed because they have no symptoms.
- Stage G3a: eGFR 45-59 - Mild to moderate loss. This is where things start getting serious. About 1 in 5 adults over 65 fall into this range, but not all have progressive disease.
- Stage G3b: eGFR 30-44 - Moderate to severe loss. Your risk of moving to kidney failure jumps sharply here. People in this stage are 2.6 times more likely to need dialysis within five years than those in G3a.
- Stage G4: eGFR 15-29 - Severe loss. You’re now in the danger zone. Specialist care is essential. Preparations for dialysis or transplant begin.
- Stage G5: eGFR under 15 - Kidney failure. Your kidneys are barely working. Without dialysis or a transplant, you won’t survive.
Albuminuria: The Silent Red Flag
eGFR alone doesn’t tell the full story. That’s where albuminuria comes in. This measures how much protein (albumin) is leaking into your urine. Healthy kidneys don’t let protein escape. If it’s there, your filters are broken. The levels are split into three categories:- A1: Less than 3 mg/mmol - Normal to mildly increased. Low risk.
- A2: 3-30 mg/mmol - Moderately increased. You’re at higher risk of heart disease and kidney decline.
- A3: Over 30 mg/mmol - Severely increased. This is a major red flag. People with A3 albuminuria have over five times the risk of dying early, even if their eGFR is still in the normal range.

Why Most People Don’t Know They Have CKD
You can have Stage G2 or G3 and feel completely fine. That’s the cruel trick of CKD. Symptoms like fatigue, swelling, or trouble sleeping only show up when damage is advanced. A 2022 survey by the National Kidney Foundation found that 78% of people diagnosed with CKD had no symptoms at all. Most found out during routine blood tests - for a knee surgery, a checkup, or managing diabetes. One patient, a nurse, only learned she had CKD when protein showed up in her urine after a routine physical. She blamed her ankle swelling on standing all day. Another man, diabetic for years, didn’t get tested until his eGFR hit 19. By then, it was too late to avoid dialysis. The problem isn’t just lack of symptoms. It’s lack of testing. The National Institute of Diabetes and Digestive and Kidney Diseases says 90% of people with CKD are undiagnosed. Why? Because doctors don’t always order the right tests - or they don’t know how to interpret them.Who Gets Tested - and Who Doesn’t
Not everyone needs routine kidney screening. But if you have any of these, you should be checked every year:- Diabetes (type 1 or 2)
- High blood pressure
- Heart disease
- Family history of kidney failure
- Obesity
- Age over 60
- Being African American, Native American, or Hispanic
How Doctors Diagnose CKD - And Common Mistakes
Diagnosis isn’t just one test. It’s two abnormal results, at least 90 days apart. Why? Because a single low eGFR could be from dehydration, infection, or medication - not permanent damage. The test you need:- Blood test: Measures creatinine to calculate eGFR. The latest CKD-EPI 2021 equation removed race adjustments - a big step toward fairness.
- Urine test: First-morning sample for albumin-to-creatinine ratio (ACR). No fancy collection needed.
Early Detection Saves Money - and Lives
Medicare spends $48 billion a year on dialysis and transplant care for end-stage kidney disease. That number is projected to hit $72 billion by 2030 if nothing changes. But early detection changes the math. A 2022 Cleveland Clinic study showed that when electronic health records flagged patients with eGFR under 60 and protein in urine, diagnosis rates jumped from 42% to 79%. Those patients got care sooner. They lived longer. They spent less on emergency care. Community screening programs are now being tested. In Baltimore, mobile units tested 5,832 adults. They found 1,247 people with CKD - 43% of them in Stage G1 or G2. That’s over a thousand people who now have a chance to avoid dialysis.What You Can Do - Right Now
You don’t need to wait for your doctor to bring it up. If you’re in a high-risk group, ask for two simple tests:- Ask for your eGFR - don’t just accept a creatinine number.
- Ask for a urine ACR test - it’s cheap, fast, and tells you more than blood alone.
- Control your blood pressure (target under 130/80).
- Manage your blood sugar if you’re diabetic.
- Stop smoking.
- Avoid NSAIDs like ibuprofen or naproxen - they hurt kidneys.
- Work with your doctor on diet. Less salt. Less processed food.
The Future: AI, Genetics, and Better Tools
The field is moving fast. In 2023, the FDA approved the first AI tool - AION nephroTM - that predicts kidney decline with 88.7% accuracy by analyzing 27 data points. It’s not replacing doctors. It’s helping them spot risk earlier. Research is also looking at genetic risk scores. A 2023 study found that 17 specific genes can predict how fast someone’s kidney function will drop - with 92% accuracy. Within five years, your DNA might help tailor your treatment plan. But none of this matters if we don’t test. If we don’t look. If we wait for symptoms. Your kidneys don’t shout. They whisper. And if you don’t listen - you might never hear them again.Can chronic kidney disease be reversed?
Early-stage CKD (Stages G1-G3a) can often be stabilized or even improved with proper management - especially if the cause is high blood pressure or diabetes. Medications like ACE inhibitors, strict blood sugar control, and lifestyle changes can slow or halt damage. But once significant scarring occurs, the damage is permanent. The goal isn’t always reversal - it’s preventing progression to kidney failure.
Do I need to see a kidney specialist right away if I’m in Stage G3?
Not always. If you’re in Stage G3a with low albuminuria (A1) and stable eGFR, your primary care doctor can manage you with annual checkups. But if your albuminuria is A2 or A3, or your eGFR is dropping fast (more than 5 mL/min/year), you should be referred to a nephrologist. That’s when targeted treatment makes the biggest difference.
Is a low eGFR always a sign of kidney disease in older adults?
No. About 40% of adults over 70 have eGFR below 60 simply because aging reduces kidney function - not because they have progressive disease. Doctors now look at trends over time and albuminuria levels to tell the difference. A stable low eGFR with no protein in urine and no other risk factors may not require treatment - just monitoring.
Can I check my kidney health at home?
You can’t measure eGFR at home - it requires a blood test. But some at-home urine strips can detect protein, which may signal early kidney damage. These aren’t diagnostic tools, but if you’re high-risk and see persistent protein on a strip, it’s a signal to get your doctor to order a proper ACR test. Don’t rely on them alone.
What’s the difference between CKD and acute kidney injury?
Acute kidney injury (AKI) is sudden - often from dehydration, infection, or a drug reaction. It can be reversible. CKD is long-term damage that lasts three months or more. AKI can lead to CKD if it happens repeatedly or isn’t treated. That’s why doctors repeat tests: to tell if a low eGFR is temporary or permanent.
Does drinking more water help my kidneys?
For most people with CKD, drinking extra water won’t improve kidney function. In fact, forcing fluids can be harmful if you have advanced disease and fluid retention. The key is staying hydrated - not overhydrated. Drink when you’re thirsty. Avoid sugary drinks and excessive salt. Your doctor will tell you if you need fluid limits.
jefferson fernandes
January 13, 2026 AT 19:31Look, I get it - kidneys are silent killers, but why do we keep acting like this is some new revelation? I’ve been telling my patients for years: if you’re diabetic or hypertensive, get your eGFR and ACR every year - no excuses. And stop relying on creatinine alone; it’s 1990s thinking. The CKD-EPI 2021 equation? Finally got rid of the race adjustment. That’s progress. But if your doctor doesn’t order the urine ACR, ask for it. Like, right now. Don’t wait for swelling. Don’t wait for fatigue. Your kidneys aren’t screaming - they’re whispering. And if you’re not listening, you’re already behind.
Pankaj Singh
January 15, 2026 AT 03:04Typical American medical propaganda. You people act like CKD is some mystery when it’s just the inevitable result of eating processed junk, sugar, and sitting on your ass all day. No one in India needs a 12-page guide to tell them kidneys fail from diabetes - we see it every day in our clinics. The real problem? You have $48 billion to waste on dialysis but won’t spend $5 on public education. Fix the food system, not the lab reports.
Trevor Davis
January 16, 2026 AT 23:52Hey - I just want to say how much this post means to me. I’m 58, prediabetic, and my last bloodwork showed eGFR at 58. I thought it was just aging. But after reading this, I went back to my doctor and asked for the ACR test - turns out I’m A2. I’m terrified, but also… relieved? Like, I didn’t know I could do something. I’ve cut out soda, started walking 30 minutes a day, and stopped taking ibuprofen for my back. I don’t feel like a patient. I feel like I’m fighting back. Thank you for not sugarcoating it.
Kimberly Mitchell
January 18, 2026 AT 07:27Let’s be brutally honest: most people with CKD are either diabetic, obese, or both. The real epidemic isn’t lack of screening - it’s lack of personal responsibility. You don’t need AI tools or genetic scores. You need to stop eating Doritos and start walking. The fact that we’re spending billions on predictive algorithms while fast food chains advertise 50-cent tacos is a moral failure. This isn’t medicine - it’s triage for a society that refuses to change.
Vinaypriy Wane
January 18, 2026 AT 11:22I’ve been a nurse for 18 years. I’ve held the hands of people who just found out they’re on dialysis next week - and they had no clue their kidneys were failing. One woman cried because she thought her swollen ankles were from her job. Another man blamed his fatigue on ‘getting old.’ We don’t need more tech. We need doctors who actually talk to patients. Not just hand them a printout and say ‘follow up in six months.’ If you’re in a high-risk group - ask. Demand. Don’t wait. I’ve seen too many people lose their kidneys because no one asked the right question.
Diana Campos Ortiz
January 20, 2026 AT 01:25Just got my ACR results back - A1, eGFR 72. I’m 42, non-diabetic, but my dad had kidney failure. I’ve been scared to check for years. I’m glad I did. This post saved me from ignoring it. I’m going to start drinking more water, cutting salt, and asking my doc about ACE inhibitors next visit. Not because I’m sick - but because I want to stay healthy. Small steps. No drama. Just care.
Jesse Ibarra
January 21, 2026 AT 13:34Oh, here we go - another ‘early detection saves lives’ lecture. Meanwhile, the same system that tells you to get tested won’t cover your insurance copay for a nephrologist visit. Or your blood pressure meds. Or your low-sodium diet. And don’t get me started on how Medicaid denies ACR tests unless you’re already in Stage G4. This isn’t prevention - it’s performative medicine. They want you to feel guilty for being sick, not fix the system that made you sick. Wake up.
Scottie Baker
January 23, 2026 AT 06:40Bro. I’m 34. I drink 3 energy drinks a day. I eat fast food 5 days a week. I never thought about my kidneys. But I just Googled ‘eGFR 55’ and found out I’m in G3a. I’m not even mad - I’m just… shook. I didn’t even know what ‘albuminuria’ meant. Now I’m deleting my Uber Eats app, drinking water like it’s my job, and begging my doctor to prescribe an ACE inhibitor. I don’t want to be the guy on dialysis at 40. This hit me harder than any doctor ever did.
Anny Kaettano
January 25, 2026 AT 04:25You know what’s powerful? When someone with Stage G1 and A1 gets a referral to a dietitian - not a nephrologist. You don’t need to be scared. You need to be equipped. I’ve worked with patients who reversed their proteinuria just by cutting salt, losing 10 pounds, and getting 7 hours of sleep. It’s not magic. It’s consistency. And yes - it’s possible. You’re not broken. You’re just at a turning point. Take a breath. Ask for help. You’ve got this.