Ciprofloxacin and Theophylline: Why This Drug Pair Can Be Deadly
 Jan, 30 2026
Jan, 30 2026
Theophylline-Ciprofloxacin Interaction Calculator
This tool calculates the potential increase in theophylline levels when taking ciprofloxacin. Theophylline has a narrow therapeutic range (10-20 mg/L). Levels above 20 mg/L may cause nausea, and levels above 30 mg/L may lead to seizures.
Input Your Medication Details
One pill can push another into the danger zone
If you’re taking theophylline for COPD or asthma, and your doctor prescribes ciprofloxacin for a sinus infection or urinary tract infection, you’re at risk - even if you’ve taken both before without issues. This isn’t a rare side effect. It’s a well-known, deadly interaction that still happens far too often.
Theophylline is a bronchodilator that’s been around since the 1920s. It works by relaxing the airways, but it doesn’t take much to push it over the edge. Its therapeutic range is narrow: 10 to 20 mg/L in the blood. Go above 20 mg/L, and you might feel nauseous. Hit 25 mg/L, and your heart could start racing or skipping beats. Cross 30 mg/L, and seizures become a real possibility. One wrong drug combo can push you from safe to life-threatening in days.
Ciprofloxacin, a fluoroquinolone antibiotic, is commonly used for infections. But it doesn’t just kill bacteria - it also shuts down a key liver enzyme called CYP1A2. That’s the same enzyme your body uses to break down theophylline. When ciprofloxacin blocks CYP1A2, theophylline doesn’t get cleared from your blood. It builds up. Slowly at first. Then fast. And you might not notice until it’s too late.
How much does the interaction actually raise the risk?
A 2011 study of over 77,000 older adults in Ontario tracked who ended up in the hospital because of theophylline toxicity. The researchers found that people taking ciprofloxacin were nearly twice as likely to be hospitalized for toxicity compared to those who weren’t. That’s not a small bump - that’s a major spike. And it wasn’t just any antibiotic. Levofloxacin? No increased risk. Amoxicillin? No risk. Trimethoprim-sulfamethoxazole? Safe. Only ciprofloxacin showed this dangerous pattern.
Why ciprofloxacin and not others? It’s about strength. Ciprofloxacin is one of the most potent inhibitors of CYP1A2 among antibiotics. Studies show it can reduce theophylline clearance by up to 50%. That means if you were normally clearing theophylline at 2.3 liters per hour, ciprofloxacin can drop that to 0.8 liters per hour - less than half. And the higher the dose of ciprofloxacin, the worse it gets. A 750 mg twice-daily dose causes about 50% more inhibition than the 500 mg version.
The U.S. Food and Drug Administration added a black box warning to ciprofloxacin labels in 1994 - the strongest warning they have. It says: monitor theophylline levels and reduce the dose by at least 33%. But many doctors still miss it. A 2017 study found that nearly 70% of electronic alerts warning about this interaction were ignored by clinicians. Why? Because they thought the infection was urgent, or because the patient had taken both drugs before. But past tolerance doesn’t guarantee safety. Your body changes. Your liver slows down. Your kidneys don’t work as well. And now, with ciprofloxacin in the mix, theophylline can climb silently.
What does toxicity actually look like?
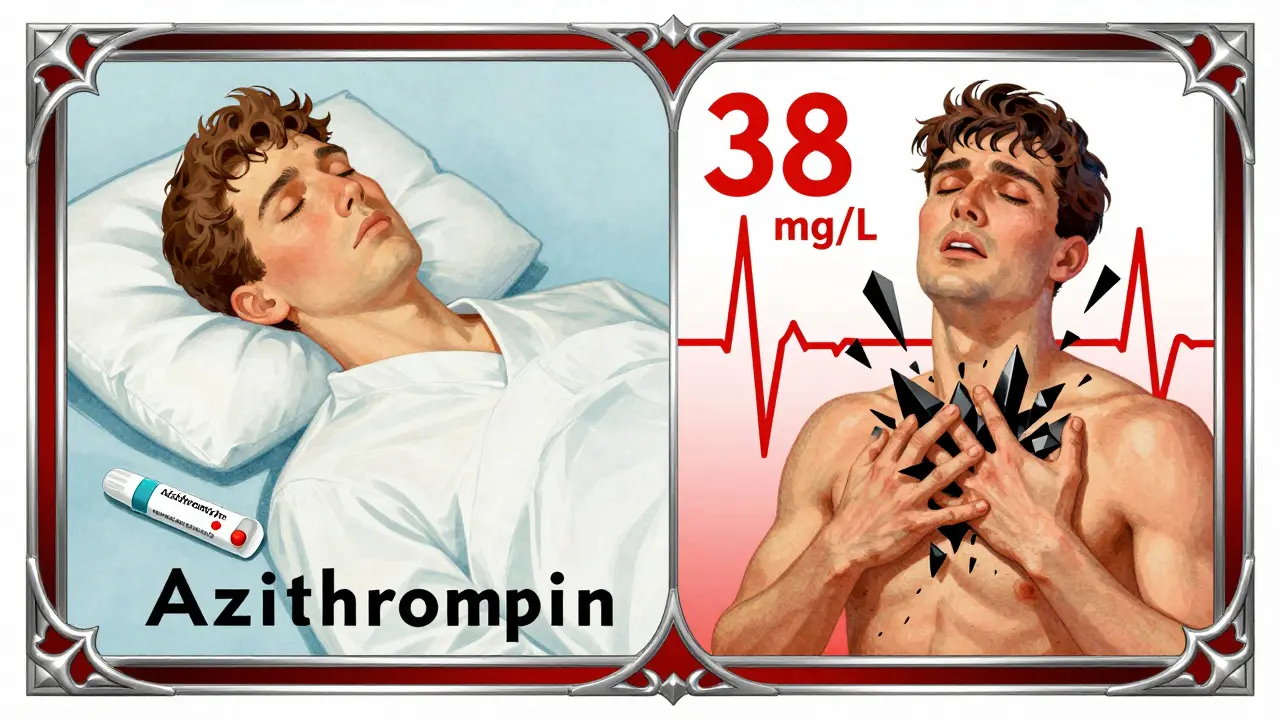
The early signs are easy to brush off. Nausea. Vomiting. Headache. Restlessness. A faster heartbeat. These aren’t dramatic. They’re the kind of things people blame on a bad stomach bug or stress. But in someone taking theophylline, they’re red flags.
By the time someone starts trembling, having palpitations, or feeling confused, the theophylline level may already be above 25 mg/L. At that point, the heart is under strain. Arrhythmias - irregular heartbeats - can turn fatal without quick intervention.
And then there’s the neurological risk. A 1990 case report described a 93-year-old woman with no history of seizures who had a grand mal seizure after starting ciprofloxacin while on theophylline. She had never had a seizure before. Her theophylline level was 38 mg/L. That’s more than double the upper limit of safety. In another study, 36% of patients on ciprofloxacin and theophylline experienced seizures. That’s more than one in three.
It’s not just about age, either. While older adults are more vulnerable - their livers clear drugs slower - younger people aren’t safe. A 2020 analysis found that 15-20% of theophylline toxicity cases in older adults are directly tied to ciprofloxacin. That’s thousands of preventable hospitalizations every year in the U.S. alone.
What should you do if you’re on both?
If you’re on theophylline and your doctor suggests ciprofloxacin, ask: Is there another option?
There are safer antibiotics. Amoxicillin-clavulanate doesn’t touch CYP1A2. Azithromycin? Minimal interaction. Levofloxacin? Only a 10-15% increase in theophylline levels - far less dangerous. Moxifloxacin? Also low risk. These are all viable alternatives for respiratory or urinary infections.
If ciprofloxacin is truly the only choice - say, for a resistant infection - then you need a clear plan:
- Get your theophylline level checked before starting ciprofloxacin.
- Reduce your theophylline dose by 30-50% right away. Don’t wait for symptoms.
- Check your level again within 24 to 48 hours after starting ciprofloxacin.
- Watch for nausea, vomiting, rapid heartbeat, tremors, or confusion. Call your doctor immediately if they appear.
- Continue monitoring levels every few days until ciprofloxacin is finished.
Many patients don’t realize they need blood tests. They think, “I’ve been on this pill for years - it’s fine.” But ciprofloxacin changes everything. Even if you’ve taken it before without issue, your body’s ability to process theophylline can change with age, illness, or other medications.
Why do doctors still miss this?
It’s not ignorance. It’s complexity. A patient with COPD might have five other conditions. They’re on six medications. The doctor’s focus is on treating the infection - fast. The alert pops up, they click through, and override it because “the patient’s been stable.” But stability doesn’t mean safety when a new drug enters the mix.
Electronic health records flag this interaction. But alerts are noisy. Clinicians get hundreds a week. Many start ignoring them. And the biggest override reason? Perceived urgency. “I need to treat this pneumonia now.” But if you treat it with ciprofloxacin, you might send the patient into the ICU.
A 2018 study found that 12.7% of older adults on theophylline still got ciprofloxacin. That’s more than one in eight. That’s not a mistake. That’s a systemic failure.
What about genetics?
Not everyone reacts the same way. Some people have a genetic variation in the CYP1A2 enzyme called CYP1A2*1F. People with this variant break down theophylline more slowly to begin with. When ciprofloxacin hits, their clearance drops by 65% - far more than average. Researchers at the University of Toronto are now testing whether genetic testing could help predict who’s at highest risk. In the future, a simple saliva test might tell you if you’re in the high-risk group.
But you don’t need to wait for genetic testing. If you’re over 65, if you’ve ever had a heart rhythm problem, if you’ve ever felt shaky or nauseated on theophylline - you’re already in a higher-risk group. Treat this interaction like a landmine. Don’t walk near it.
What’s the bottom line?
This isn’t a hypothetical risk. It’s a proven, deadly interaction with decades of evidence behind it. Theophylline and ciprofloxacin shouldn’t be used together unless there’s no other choice - and even then, only with strict monitoring and a dose reduction.
If you’re on theophylline:
- Never start ciprofloxacin without talking to your doctor or pharmacist.
- Ask: “Is there a safer antibiotic?”
- If ciprofloxacin is unavoidable, demand a blood test before and after starting it.
- Know the early signs of toxicity: nausea, vomiting, fast heartbeat, shaking.
- Don’t assume past tolerance means future safety.
Every year, thousands of people are hospitalized because of this interaction. Most of those cases are preventable. You don’t need to be one of them.
Diksha Srivastava
January 31, 2026 AT 11:22Sidhanth SY
February 2, 2026 AT 08:11Blair Kelly
February 2, 2026 AT 23:56Rohit Kumar
February 4, 2026 AT 22:07Lily Steele
February 6, 2026 AT 03:15Marc Bains
February 8, 2026 AT 01:21Darren Gormley
February 8, 2026 AT 07:31Mike Rose
February 8, 2026 AT 19:19Russ Kelemen
February 10, 2026 AT 04:15Beth Cooper
February 11, 2026 AT 23:35Donna Fleetwood
February 12, 2026 AT 15:54Melissa Cogswell
February 13, 2026 AT 21:09