Compare Hsquin (Hydroxychloroquine) with Alternatives for Autoimmune and Inflammatory Conditions
 Nov, 3 2025
Nov, 3 2025
Autoimmune Treatment Comparison Tool
Compare Your Treatment Options
Select your condition and priorities to see which treatment might be most suitable for you.
Hydroxychloroquine - sold under the brand name Hsquin - was once widely used for malaria and later became a go-to drug for autoimmune conditions like lupus and rheumatoid arthritis. But after years of controversy, shifting guidelines, and new research, many patients and doctors are asking: Are there better options? If you’re on Hsquin or considering it, you deserve to know what else is out there - and what actually works today.
What Hsquin (hydroxychloroquine) actually does
Hydroxychloroquine is an antimalarial drug that also has immune-modulating effects. It doesn’t cure autoimmune diseases, but it helps calm overactive immune responses. For people with systemic lupus erythematosus (SLE), it reduces skin rashes, joint pain, and fatigue. In rheumatoid arthritis, it slows joint damage and lowers flare frequency. It’s often used long-term because it’s generally well-tolerated and doesn’t suppress the immune system as hard as steroids or biologics.
But here’s the catch: it’s not magic. Studies show only about 40-60% of lupus patients respond well to hydroxychloroquine alone. And it takes weeks - sometimes months - to see results. That’s why many doctors pair it with other drugs, or switch entirely if side effects show up.
Common side effects of Hsquin
Most people tolerate hydroxychloroquine fine. But side effects can be serious - and they don’t always show up right away.
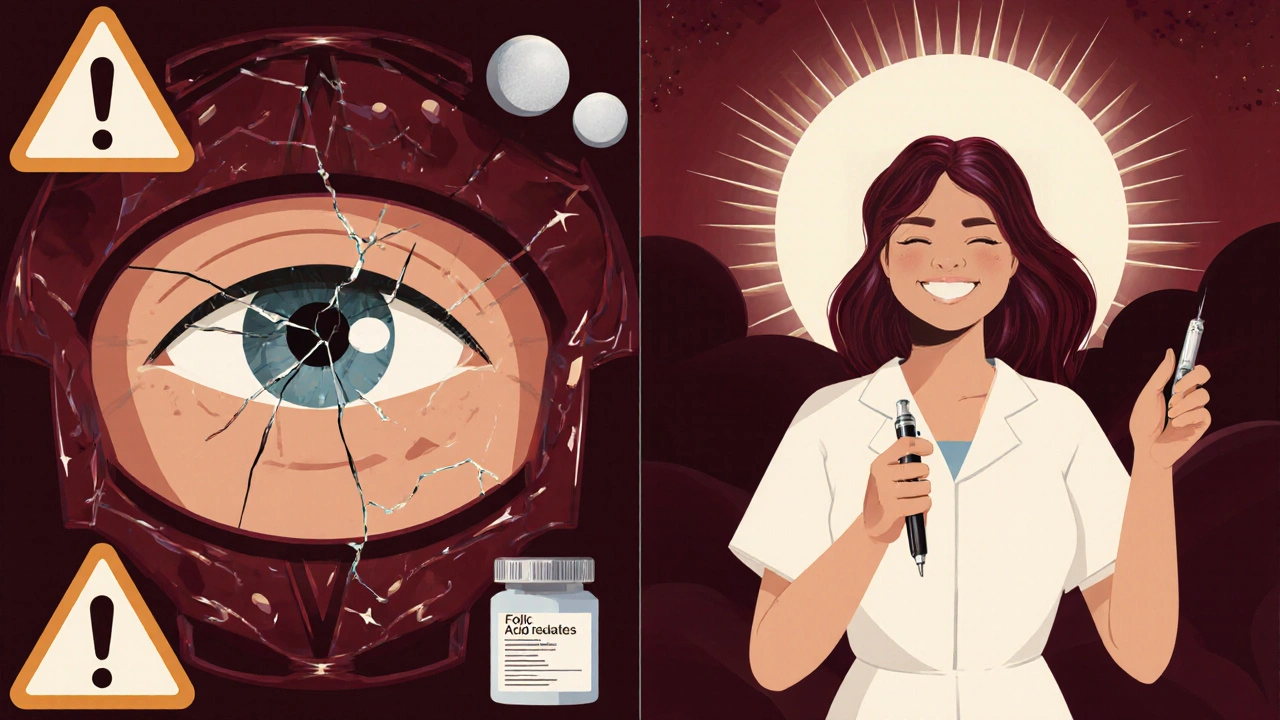
- Eye damage (retinopathy): Risk increases after 5+ years of use. Requires annual eye exams.
- Stomach upset: Nausea, diarrhea, cramps - common early on.
- Headaches and dizziness.
- Low blood sugar: Especially risky for diabetics.
- Heart rhythm issues: Rare, but dangerous. Can cause QT prolongation, especially with other drugs.
The FDA issued a warning in 2020 about heart risks when combined with azithromycin - a combo that briefly gained attention during the pandemic. Even without that, long-term use demands monitoring. If you’re on Hsquin, you should have an eye exam every year and an ECG if you have heart disease or take other QT-prolonging meds.
Alternative 1: Chloroquine
Chloroquine is hydroxychloroquine’s older cousin. It works similarly but is stronger and more toxic. It’s rarely used today for autoimmune conditions because it carries a higher risk of retinal damage - up to twice as much as hydroxychloroquine.
Chloroquine is still used in some parts of the world for malaria, but for lupus or arthritis, it’s not the first choice anymore. If your doctor suggests it, ask why. In most cases, hydroxychloroquine is safer and just as effective.
Alternative 2: Sulfasalazine
Sulfasalazine is an old-school drug originally developed for ulcerative colitis. It’s now commonly used for rheumatoid arthritis and sometimes for lupus-related joint pain. It works by reducing inflammation in the gut and joints.
Pros:
- Lower risk of eye damage
- Good for patients with both arthritis and inflammatory bowel disease
- Cost-effective
Cons:
- Can cause nausea, headaches, and low sperm count in men
- Turns urine and tears orange - which freaks people out at first
- Slower to work than hydroxychloroquine
It’s not a direct replacement for Hsquin, but for patients who can’t tolerate eye monitoring or need gut-targeted therapy, sulfasalazine is a solid backup.

Alternative 3: Methotrexate
Methotrexate is the most common disease-modifying antirheumatic drug (DMARD) used for rheumatoid arthritis. It’s stronger than hydroxychloroquine and works faster - often within 6-8 weeks.
For lupus patients, methotrexate is used when skin or joint symptoms don’t respond to hydroxychloroquine alone. It’s also used in combination with Hsquin for better control.
Pros:
- Proven to prevent joint damage
- Works well with hydroxychloroquine
- Available as a weekly pill or injection
Cons:
- Requires monthly blood tests (liver and kidney function)
- Can cause mouth sores, fatigue, and hair thinning
- Not safe during pregnancy
- Must take folic acid daily to reduce side effects
Methotrexate isn’t for everyone, but for moderate to severe arthritis or lupus with organ involvement, it’s often the next step after hydroxychloroquine.
Alternative 4: Leflunomide
Leflunomide is another DMARD used for rheumatoid arthritis. It blocks immune cells that cause joint inflammation. It’s less commonly used for lupus but can be helpful when methotrexate fails or isn’t tolerated.
Pros:
- Once-daily pill
- Effective for joint swelling and pain
- Can be used if methotrexate causes liver issues
Cons:
- High risk of liver toxicity
- Can cause diarrhea, high blood pressure, and hair loss
- Stays in the body for months - requires a special washout if you need to stop it
Leflunomide is a good option if you’ve tried hydroxychloroquine and methotrexate and still have active disease. But it’s not a first-line replacement - more of a second or third choice.
Alternative 5: Biologics (like belimumab or rituximab)
For lupus patients who don’t respond to traditional drugs, biologics are the next level. Belimumab (Benlysta) is the only FDA-approved biologic specifically for lupus. It targets B-cells that drive autoimmune attacks.
It’s given as a monthly IV infusion or weekly injection. Studies show it reduces flares by about 30% and lowers steroid use.
Rituximab (Rituxan) isn’t officially approved for lupus but is used off-label for severe cases - especially kidney or neurological involvement.
Pros:
- Targets the root cause of lupus, not just symptoms
- Can induce remission in resistant cases
- Lower long-term steroid use
Cons:
- Expensive - often over $20,000 per year
- Requires IV infusions or injections
- Higher infection risk
- Not always covered by insurance without trial of other drugs first
Biologics aren’t replacements for Hsquin - they’re for when Hsquin isn’t enough. Most patients try hydroxychloroquine, then methotrexate, then biologics.
When to consider stopping Hsquin
You shouldn’t quit Hsquin on your own. But if you’re experiencing:
- Vision changes (blurriness, light sensitivity, blind spots)
- Unexplained heart palpitations or dizziness
- Severe nausea or skin rashes
- Low blood sugar you can’t explain
…then talk to your doctor. You might need a switch. Some patients stop because of cost - Hsquin can be expensive without insurance. Others stop because they feel fine and think they don’t need it anymore. That’s risky. Stopping suddenly can trigger a flare.
What most doctors recommend today
In 2025, the standard approach is:
- Start with hydroxychloroquine for mild lupus or arthritis.
- Get annual eye exams - don’t skip them.
- If symptoms persist after 3-6 months, add methotrexate or switch to sulfasalazine.
- If you still have flares or organ damage, move to biologics like belimumab.
- Avoid chloroquine unless there’s no other option.
There’s no one-size-fits-all. Your choice depends on your symptoms, other health conditions, cost, and how well you tolerate side effects.
Real patient stories
Anna, 52, from Durban, was on Hsquin for 7 years for lupus. Her vision started blurring. Her eye doctor caught early retinopathy. She switched to methotrexate and now takes folic acid daily. Her joints still ache, but her eyes are stable.
James, 38, had rheumatoid arthritis. Hsquin helped a little, but he still couldn’t grip his tools. His doctor added sulfasalazine. The orange urine freaked him out at first - but within 3 months, he could lift his kids again.
These aren’t rare cases. They’re routine.
Bottom line
Hsquin isn’t bad - it’s just not always enough. For many, it’s a helpful first step. But if it’s not working, or if you’re worried about side effects, there are real, proven alternatives. The key is not to stay stuck on one drug. Autoimmune diseases change. Your treatment should too.
Don’t be afraid to ask your doctor: "Is Hsquin still the best option for me?" If they don’t have a clear answer, get a second opinion. Your health isn’t a one-drug solution.
Is hydroxychloroquine still used for lupus in 2025?
Yes, but not as the only treatment. Hydroxychloroquine is still a first-line option for mild lupus because it reduces flares and protects organs over time. However, doctors now combine it with other drugs like methotrexate or move to biologics faster if symptoms are severe. It’s no longer the default for everyone.
Can I switch from Hsquin to sulfasalazine safely?
Yes, many patients do. Sulfasalazine is a good alternative if you’re concerned about eye damage or if you have inflammatory bowel disease along with arthritis. Your doctor will likely overlap the two drugs for 2-4 weeks to avoid a flare, then slowly taper Hsquin. Blood tests are needed to monitor liver function.
Why is methotrexate often paired with hydroxychloroquine?
They work differently. Hydroxychloroquine calms the immune system broadly, while methotrexate targets specific inflammatory cells. Together, they’re more effective than either alone - especially for joint damage in rheumatoid arthritis. Studies show patients on both drugs have fewer flares and less need for steroids.
Are natural alternatives like turmeric or fish oil effective?
Turmeric and omega-3s may help reduce inflammation slightly and improve overall wellness, but they are not replacements for prescription drugs. No study shows they prevent joint damage or control lupus flares like hydroxychloroquine or methotrexate do. They can be used as supplements, but never instead of medical treatment.
What’s the biggest mistake people make when switching from Hsquin?
Stopping Hsquin cold turkey without starting the next drug. Hydroxychloroquine stays in your system for weeks. If you stop it and don’t replace it, your immune system can rebound hard - leading to a severe flare. Always work with your doctor to transition slowly and monitor symptoms.
Lexi Brinkley
November 5, 2025 AT 13:20Orange urine?? 😱 I’d think I was dying lol. But honestly, if it gets me back to lifting my kids? Worth it. 🙌
Brad Seymour
November 6, 2025 AT 00:57Love this breakdown. So many people just panic and quit Hsquin without realizing how gradual the taper needs to be. You’re right-flares don’t wait for your schedule. Thanks for the clarity.
Malia Blom
November 7, 2025 AT 22:51Let’s be real-hydroxychloroquine was always a Band-Aid on a bullet wound. The fact that we’re still debating its "effectiveness" in 2025 is a symptom of a broken medical system that clings to old drugs because they’re cheap, not because they’re good. We’re treating symptoms like they’re the disease. 🤷♀️
Abigail Chrisma
November 9, 2025 AT 11:32As someone who’s been on methotrexate for 10 years with lupus-yes, the hair thinning sucks. The mouth sores? Brutal. But I can walk without crying. And yes, I take folic acid like it’s my job. If you’re scared of side effects, talk to your rheumatologist-not Reddit. But also, yes, this post nails the progression path. 🙏
Steve Phillips
November 11, 2025 AT 02:09Oh, please. Sulfasalazine? That’s like swapping a Tesla for a 1998 Corolla with duct tape on the door. Hydroxychloroquine may have retinopathy risks-but at least it doesn’t make you smell like a citrus factory. And don’t get me started on leflunomide-"stays in your system for months"? That’s not a feature, that’s a biohazard. The fact that anyone still considers this a "viable alternative" is laughable. Methotrexate? Fine. Biologics? Fine. But sulfasalazine? Please. I’ve seen patients on it for 2 years and still can’t button their shirts. It’s not a replacement-it’s a consolation prize.
And don’t even get me started on "natural alternatives." Turmeric? Please. If you think a spice can stop your immune system from eating your joints, you’ve been scrolling TikTok too long. This isn’t yoga class, it’s immunology. We’re not curing arthritis with smoothies. We’re managing a systemic autoimmune disorder with pharmacology. If you’re looking for "natural," go hug a tree. But don’t confuse wellness trends with science.
And the "orange urine" thing? That’s not a side effect-that’s a warning label in neon. If you’re not horrified by that, you’re not paying attention. I’ve had patients panic because they thought they were bleeding internally. It’s not cute. It’s a red flag. And yet, here we are, treating it like a quirky Instagram filter.
Biologics are expensive? So is a wheelchair. So is a kidney transplant. So is losing your vision. You don’t get to pick your disease’s price tag. If your insurance won’t cover belimumab, fight them. Go to your congressman. Write letters. But don’t settle for a drug that’s half as effective just because it’s cheaper. That’s not pragmatism-that’s surrender.
And for the love of God, stop calling hydroxychloroquine "bad." It’s not bad-it’s imperfect. It’s the first tool in a toolbox that’s been neglected for decades. The problem isn’t the drug-it’s the lack of investment in alternatives. We’ve had the same DMARDs since the 80s. We need innovation, not nostalgia.
And yes-I’ve seen retinopathy. I’ve seen QT prolongation. I’ve seen patients on Hsquin for 12 years and still walking. It’s not magic. But it’s not evil either. It’s a tool. Use it wisely. Monitor it. Don’t demonize it. And for heaven’s sake, stop pretending that the only way forward is to trash everything that came before you. Medicine isn’t a cult. It’s a science. And science doesn’t throw out the baby because the bathwater’s a little warm.
Edward Weaver
November 12, 2025 AT 06:00Biologics cost $20K? That’s why America’s healthcare system is a joke. In other countries, this stuff is covered. Here? You need to be rich or have a miracle insurance plan. Meanwhile, my cousin in Canada gets her biologic for free. We’re not better at medicine-we’re just better at profiting off suffering.
Erika Puhan
November 13, 2025 AT 17:20Let’s address the elephant in the room: hydroxychloroquine was weaponized during the pandemic. That’s why people are so quick to dismiss it now. But correlation ≠ causation. Just because it was politicized doesn’t mean the science is invalid. The retinopathy risk is real-but so is the data showing reduced mortality in SLE patients on long-term HCQ. The problem isn’t the drug. It’s the narrative. And we’re all just shouting louder now instead of listening.
Ankit Yadav
November 14, 2025 AT 00:57For those in India or lower-income regions-HCQ is still a lifeline. It’s cheap. It’s accessible. Yes, monitoring is ideal-but not always possible. We don’t have annual eye exams for everyone. So we use what works. And for many, it does. This isn’t about perfection. It’s about survival. Don’t judge a treatment by the privileges of Western clinics.
Rachel Puno
November 15, 2025 AT 15:12My mom switched from HCQ to methotrexate last year. She was terrified. But now? She’s gardening again. She says the folic acid is her new best friend. Don’t fear change-embrace the next step. You’re not failing if you need more than one drug. You’re fighting smart.
Meghan Rose
November 17, 2025 AT 10:12Wait-so if I’m on HCQ and I don’t get eye exams, I’m just… ignoring my body? And you’re telling me I should feel guilty? But what if I can’t afford the exam? Or I’m uninsured? Or I’m just… tired? Is the solution to make me feel worse for not being perfect? This post feels like a guilt trip dressed as advice.