Drug Allergies vs. Side Effects: How to Tell Them Apart and Stay Safe
 Nov, 18 2025
Nov, 18 2025
It’s easy to assume that if you feel sick after taking a pill, it’s an allergy. But that’s not always true - and mixing up the two can put your health at risk. Every year, millions of people avoid life-saving medications because they think they’re allergic when they’re really just experiencing a common side effect. The difference isn’t just semantics - it’s safety, cost, and sometimes, life or death.
What’s Really Happening in Your Body?
A drug allergy means your immune system has mistaken a medication for a threat - like a virus or pollen - and launched a full attack. This triggers histamine release, inflammation, and potentially dangerous symptoms like hives, swelling, or anaphylaxis. It’s not about how the drug works; it’s about your body’s wrong response to it.
Side effects, on the other hand, are built into the drug’s chemistry. They’re predictable. For example, antibiotics like amoxicillin can cause diarrhea because they kill good bacteria in your gut. Statins can cause muscle aches because they interfere with muscle cell energy production. These aren’t immune reactions. They’re side effects - and they often get better over time or with dose adjustments.
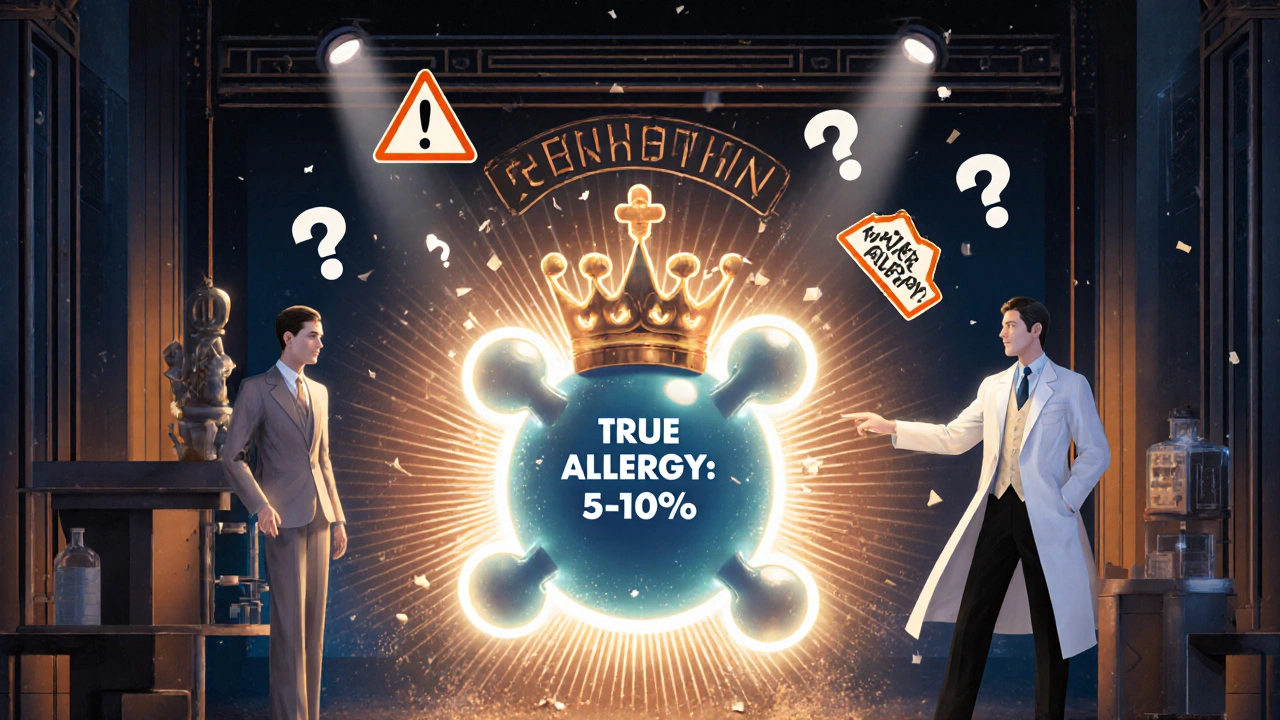
Here’s the scary part: only 5 to 10% of reported drug reactions are true allergies. That means 9 out of 10 people who say they’re allergic to penicillin, sulfa, or other common drugs aren’t. They’re just reacting to a known side effect.
Timing Tells the Story
One of the clearest ways to tell the difference is when the reaction happens.
If you break out in hives, your throat swells, or you feel dizzy within minutes to an hour after taking a pill - especially with penicillin or cephalosporins - that’s a red flag for an IgE-mediated allergic reaction. These can escalate fast. Anaphylaxis is rare but deadly, and it demands immediate treatment.
But if you feel nauseous, get a headache, or have mild diarrhea 12 to 72 hours after starting a new medication, that’s almost always a side effect. These often fade as your body adjusts. For instance, metformin causes stomach upset in 20-30% of users, but most people tolerate it after a few weeks.
Delayed reactions are trickier. A rash that appears 10 to 14 days after starting amoxicillin might look like an allergy - but if you had a virus at the same time (like mono or Epstein-Barr), it’s likely just a viral rash mislabeled as an allergy. Studies show up to 90% of these cases in kids are misdiagnosed.
Real Examples People Get Wrong
Let’s look at real cases:
- Penicillin allergy: A patient says, “I broke out in a rash when I took penicillin as a child.” But the rash was from a viral infection, not the drug. Decades later, they’re stuck with stronger, costlier antibiotics - and at higher risk of C. diff infection.
- Statins: “I stopped my cholesterol pill because my muscles hurt.” That’s a known side effect. Most people can switch to another statin or lower the dose. But if they think it’s an allergy, they avoid all cholesterol meds - increasing heart attack risk.
- Sulfa drugs: “I’m allergic to sulfa.” But the reaction was actually nausea and dizziness - common side effects. Now they can’t get a safe UTI treatment, so they get recurrent infections.
- NSAIDs: “I get stomach pain with ibuprofen.” That’s not an allergy. It’s irritation. But if they think it’s an allergy, they might avoid all pain relievers, including acetaminophen, which is safer for them.
These aren’t rare stories. In fact, 15-20% of hospitalized patients have a documented drug allergy - but up to 95% of those labeled as penicillin-allergic can safely take it after proper testing.
Why Mislabeling Costs Lives - and Money
When doctors think you’re allergic to penicillin, they reach for vancomycin, clindamycin, or fluoroquinolones instead. These drugs are broader-spectrum, more expensive, and more likely to cause antibiotic-resistant infections.
Patients with a mislabeled penicillin allergy have a 2.5 times higher risk of getting C. diff - a severe, sometimes fatal gut infection. They also pay $1,000 more per hospital stay on average.
Across the U.S., this one mistake costs over $1 billion a year. In South Africa and other low-resource settings, it’s worse. People miss out on effective treatments because doctors don’t have the tools to test for true allergies.
And it’s not just about money. It’s about access. A woman in Durban was denied antibiotics for a urinary tract infection for three years because she thought she was allergic to sulfa. She ended up with kidney damage. Her reaction? Nausea - a side effect, not an allergy.
How to Know for Sure
If you think you have a drug allergy, don’t just accept it. Ask these questions:
- What exactly happened? (Rash? Swelling? Trouble breathing? Nausea?)
- When did it happen? (Within an hour? After a week?)
- Did you have an infection or virus at the same time?
- Did you take the same drug again and have the same reaction?
Then talk to your doctor about referral to an allergist. For penicillin, skin testing is 97-99% accurate. A simple scratch test followed by a small oral dose under supervision can confirm if you’re truly allergic.
Most people who think they’re allergic to penicillin - even those with a history of rash - pass the test. And if you’re cleared, you can safely use cheaper, more effective antibiotics for the rest of your life.

What You Can Do Today
You don’t need to wait for a doctor’s appointment to start getting this right.
- Update your medication list. Don’t just write “allergic to penicillin.” Write: “Rash after amoxicillin at age 8 - never rechallenged.”
- Ask your pharmacist: “Is this reaction likely an allergy or a side effect?” Pharmacists are trained to spot the difference.
- Use patient tools like the American College of Physicians’ “Allergy vs. Side Effect” guide. It’s free and helps you describe your reaction accurately.
- If you’ve been told you’re allergic to a common drug like penicillin, sulfa, or NSAIDs, ask: “Can I be tested?”
Many hospitals now have pharmacist-led allergy assessment programs. In the U.S. Veterans Health system, these programs cut inappropriate penicillin avoidance by 80%. That’s not magic - it’s better information.
The Bigger Picture
This isn’t just about one drug or one reaction. It’s about how we think about medicine. We’ve been taught to fear all bad reactions - but not all reactions are created equal.
True drug allergies are rare. They need to be taken seriously. But side effects? They’re part of the deal with many medications. And they’re often manageable.
By learning to tell the difference, you protect yourself from unnecessary risks. You avoid dangerous alternatives. You save money. And you make sure you get the best possible treatment - not just the safest one.
Next time you’re told you’re allergic to a drug, don’t just nod. Ask: “Is this really an allergy? Or could it be something else?”
Can you outgrow a drug allergy?
Yes, especially with penicillin. Up to 80% of people who had a penicillin allergy as a child lose it over time - even if they never got tested. The immune system changes. But without retesting, you’ll never know. That’s why doctors recommend evaluation if you were labeled allergic more than 10 years ago.
Is a rash always a sign of allergy?
No. Many rashes from antibiotics - especially amoxicillin - happen because of a virus, not the drug. In fact, up to 90% of rashes in children on amoxicillin with a cold or flu are mislabeled as allergies. The rash is harmless and fades on its own. Testing can confirm whether it’s truly an immune reaction.
Can side effects turn into allergies?
No. Side effects and allergies are different mechanisms. A side effect won’t become an allergy. But you can develop a true allergy to a drug you’ve taken before without any prior reaction. That’s rare, though. Most people who think they’ve developed an allergy after repeated use are actually experiencing worsening side effects - not an immune response.
What should I do if I think I had an allergic reaction?
Stop the drug immediately. If you have trouble breathing, swelling of the face or throat, or feel faint - call emergency services. Afterward, see an allergist for testing. Don’t rely on a past label. Write down exactly what happened: timing, symptoms, and treatment. This helps avoid misdiagnosis later.
Are there tests for all drug allergies?
No. Reliable tests exist only for a few drugs - mainly penicillin and some cephalosporins. For others, like sulfa or NSAIDs, diagnosis is based on history and sometimes a supervised challenge. Blood tests for IgE are rarely helpful for most drugs. Skin tests and oral challenges remain the gold standard when available.
Can I take a drug I’m allergic to if I really need it?
Only under strict medical supervision. For life-saving drugs like certain antibiotics or chemotherapy agents, doctors may use desensitization - slowly increasing doses over hours or days to temporarily tolerate the drug. This is not for mild side effects. It’s only done in hospitals for true IgE-mediated allergies when no alternatives exist.
How can I make sure my doctor knows the difference?
Be specific in your medical records. Instead of writing “allergic to penicillin,” write: “Hives and itching 30 minutes after taking amoxicillin at age 6. No breathing trouble. Never tested.” This helps your doctor decide whether to refer you to an allergist. Ask your pharmacist to review your list - they often catch vague labels.
Kara Binning
November 19, 2025 AT 23:46So let me get this straight-we’re telling people they’re not allergic to penicillin just because they got a rash after a virus? What’s next? Telling people they’re not allergic to peanuts because they ate them at a birthday party? This is dangerous nonsense. I’ve seen people go into anaphylaxis because someone ‘thought’ it was just a side effect. Don’t play doctor with my life.
river weiss
November 21, 2025 AT 11:10It is critically important to distinguish between immune-mediated hypersensitivity reactions and pharmacologically mediated adverse effects. The former involves IgE, T-cells, or other immune effectors; the latter is a direct, dose-dependent consequence of drug pharmacology. Misclassification leads to suboptimal therapy, increased resistance, and avoidable morbidity. Documentation must reflect precise terminology: ‘suspected allergy’ versus ‘known side effect.’
Frank Dahlmeyer
November 23, 2025 AT 10:33Let me tell you something-this is the single most important public health message I’ve seen in years. I used to think I was allergic to sulfa because I got a stomachache after my UTI med back in 2010. Turns out, I was dehydrated, had a stomach bug, and the nausea was just the drug’s way of saying ‘hey, I don’t like empty bellies.’ I got tested last year, cleared, and now I’m on the cheapest, most effective antibiotic in the book. My doctor called it a ‘medical miracle.’ I call it common sense. If you’ve been avoiding a drug because of a vague reaction from 15 years ago, you owe it to yourself to get tested. It’s not a luxury-it’s a right.
Reema Al-Zaheri
November 25, 2025 AT 06:56While the article is well-structured and scientifically accurate, it fails to address the cultural context in which drug allergies are reported. In many low-income regions, patients self-diagnose allergies due to lack of access to healthcare; they associate any adverse reaction-however mild-with ‘allergy’ as a shorthand for ‘this drug made me sick.’ Without systemic education and accessible allergist services, individual awareness remains insufficient. Structural change is required, not just individual action.
Derron Vanderpoel
November 26, 2025 AT 16:03OMG I just realized-I’ve been calling myself allergic to ibuprofen for 12 years because I get a headache after taking it… but that’s literally the opposite of what it’s supposed to do?? I’ve been taking Tylenol every time I have a migraine and now I’m worried I’ve been hurting my liver?? I’m gonna call my pharmacist tomorrow. This post literally changed my life. Thank you.
Timothy Reed
November 26, 2025 AT 20:29This is an excellent resource for both patients and providers. I encourage all clinicians to incorporate routine allergy reassessment into annual medication reviews, particularly for penicillin labels. The data is clear: most reported allergies are not true allergies. Implementing pharmacist-led allergy clinics in primary care settings can reduce unnecessary antibiotic use, lower costs, and improve outcomes. This is evidence-based practice at its best.
Christopher K
November 27, 2025 AT 09:17So let me get this right-you’re telling me I’m not allergic to penicillin because I got a rash as a kid? That’s like saying I’m not allergic to cats because I sneezed once at a petting zoo. The government wants us to trust doctors more? Cool. Now give me a free skin test and a guarantee I won’t die if I take it again. Until then, I’ll keep my ‘allergy’ label. It’s my only insurance against your ‘science.’
harenee hanapi
November 28, 2025 AT 14:21Everyone’s so quick to say ‘it’s just a side effect’-but what if it’s not? What if your ‘harmless rash’ turns into Stevens-Johnson? What if your ‘nausea’ is the first sign of something worse? You’re normalizing risk. You’re making people feel guilty for being scared. And you know what? I’m not sorry for being scared. My cousin died because someone said ‘it’s probably just a side effect.’ So don’t you dare tell me to ‘just get tested.’ Not everyone has access. Not everyone has time. Not everyone has a doctor who listens.
Andy Feltus
November 29, 2025 AT 23:23It’s funny how we treat medicine like it’s a moral test. ‘You’re allergic’ becomes a badge of honor-a story we tell to prove we’ve suffered, that we’re special, that we’ve been through something. But what if the truth is simpler? What if you just had a bad day, a virus, and a drug that didn’t agree with your gut? Maybe the real danger isn’t the medicine-it’s our need to turn every discomfort into a trauma narrative. Maybe we’re allergic to uncertainty more than we’re allergic to penicillin.
Brian Rono
November 30, 2025 AT 14:48Oh, so now we’re all supposed to be amateur immunologists? You think your grandma’s ‘mild rash’ from 1978 is ‘probably’ not an allergy? That’s the same logic that led to the opioid crisis-‘it’s just a little pain, take more.’ You’re not a doctor. Your ‘study’ isn’t a gospel. And I’m not handing over my life to some algorithm that says ‘80% of people are fine.’ I’ll keep my label. It’s the only thing keeping me alive.
seamus moginie
November 30, 2025 AT 16:48Brilliant article. I work in a rural clinic in Mayo, and we see this every week. A woman comes in with a UTI, says she’s allergic to sulfa-so we give her a $500 antibiotic that makes her vomit. She leaves angry. We’re stuck. We need more funding for allergy clinics. And we need pharmacists to be the first line-not just the ones who hand out pills. This isn’t just medicine. It’s justice.
Dana Dolan
December 1, 2025 AT 21:38Wait-so I’ve been saying I’m allergic to NSAIDs because my stomach hurts… but that’s just irritation? So I can try naproxen? I’ve been taking tramadol for years because I thought ibuprofen would kill me. I’m gonna try it tomorrow. Fingers crossed.
Steve and Charlie Maidment
December 2, 2025 AT 22:07You know what’s funny? You spend all this time explaining the difference between allergies and side effects… but you never mention that the real problem is the pharmaceutical industry pushing drugs without proper long-term studies, and then the medical system refusing to admit they got it wrong. You’re blaming patients for being scared, when the system made them scared in the first place. And now you want us to trust it? After all the lies? After all the overdoses? After all the ignored warnings? No thanks. I’ll keep my ‘allergy.’ It’s the only truth I’ve got left.