Gout Attacks: Understanding Uric Acid, Triggers, and Effective Medication Strategies
 Dec, 25 2025
Dec, 25 2025
When your big toe suddenly swells up, turns bright red, and feels like it’s on fire-no matter how gently you touch it-you’re not imagining things. This is a gout attack, and it’s one of the most painful forms of arthritis. It doesn’t come out of nowhere. It builds up over years, hidden in your bloodstream, until something tips the balance. The culprit? uric acid. Too much of it, and it starts forming sharp, needle-like crystals in your joints. That’s when the pain hits.
Why Uric Acid Builds Up
Uric acid is a waste product your body makes when breaking down purines-natural substances found in many foods and your own cells. Most people’s kidneys flush it out without issue. But in gout, something goes wrong. About 90% of cases happen because the kidneys aren’t clearing uric acid properly. The rest are due to the body making too much. Either way, when blood levels climb above 6.8 mg/dL, uric acid starts crystallizing. That’s the tipping point.Humans are unusual in this. Most animals have an enzyme called uricase that breaks down uric acid into something easier to remove. We lost that gene during evolution. So we’re stuck with what we’ve got. Genetics play a big role too. Variations in genes like SLC2A9 and ABCG2 affect how your kidneys handle uric acid. If your family has a history of gout, your risk goes up significantly.
What Triggers a Gout Attack
You can have high uric acid for years without symptoms. Then, something triggers a flare. And it’s rarely just one thing.One major trigger is a sudden change in uric acid levels-whether it goes up or down. That’s why starting a medication to lower uric acid can actually cause a flare. Your body sees the crystals shifting and mistakes them for an invasion. The immune system reacts violently, sending inflammatory signals that cause swelling, heat, and unbearable pain.
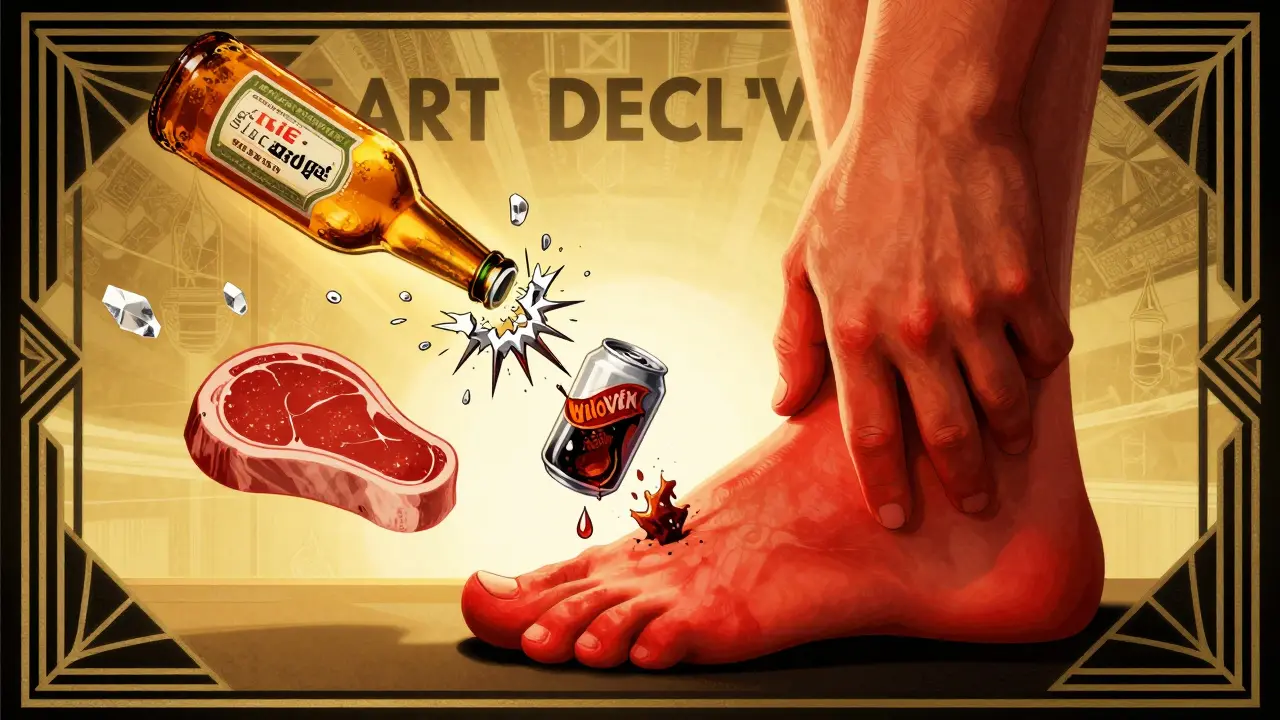
Diet plays a role, but not as simply as people think. Eating a steak or shrimp won’t instantly cause an attack. But regularly loading up on purine-rich foods-like organ meats (liver, kidneys), certain seafood (anchovies, sardines, mussels), and red meat-keeps your levels high. Alcohol, especially beer, is a double threat. It’s high in purines and also blocks uric acid excretion. A daily 12-ounce beer increases your risk by nearly 50%. Spirits are less risky, but still not safe. Wine? Less impact, but still not harmless if you drink heavily.
Fructose is another sneaky trigger. Sugary drinks-sodas, fruit juices, sweetened teas-raise uric acid by 20-30%. The body breaks down fructose in a way that depletes ATP, a key energy molecule, and that process produces more uric acid as a byproduct.
Dehydration is a silent contributor. If you’re not drinking enough water, your kidneys can’t flush uric acid effectively. Aim for at least 2 liters a day. Joint injury-even a minor bump or twist-can dislodge crystals and trigger a flare. Stress, surgery, or even rapid weight loss can do the same.
How Gout Attacks Happen Inside Your Body
It’s not just about crystals sitting in your joint. The real damage comes from your immune system’s reaction. When monosodium urate crystals form, immune cells called macrophages recognize them as foreign invaders. They activate something called the NLRP3 inflammasome-a molecular alarm system. This triggers the release of interleukin-1β, a powerful inflammatory signal. That’s what causes the redness, heat, swelling, and pain.This is why treating gout isn’t just about lowering uric acid. It’s also about calming that overactive immune response. That’s why medications like colchicine and NSAIDs work so well during flares-they interrupt this chain of inflammation.
Medications for Acute Gout Attacks
When you’re in the middle of a flare, you need fast relief. Three main options are used:- NSAIDs like indomethacin (50 mg three times a day) or naproxen. These reduce inflammation and pain quickly. But they’re not safe for people with kidney disease, stomach ulcers, or heart failure.
- Colchicine (0.6 mg every hour until symptoms improve, up to 3 doses, then 0.6 mg twice daily). It blocks the immune response triggered by crystals. Side effects? Diarrhea, nausea, vomiting. Dosing must be lowered if you have kidney problems.
- Corticosteroids like prednisone (30-40 mg daily for 5 days, then tapered). These are used when NSAIDs or colchicine aren’t an option. They can be taken orally or injected directly into the joint.
Don’t wait to treat a flare. The sooner you start, the faster it fades. Delaying treatment can make the attack last longer and increase the chance of it spreading to other joints.
Long-Term Gout Management: Lowering Uric Acid for Life
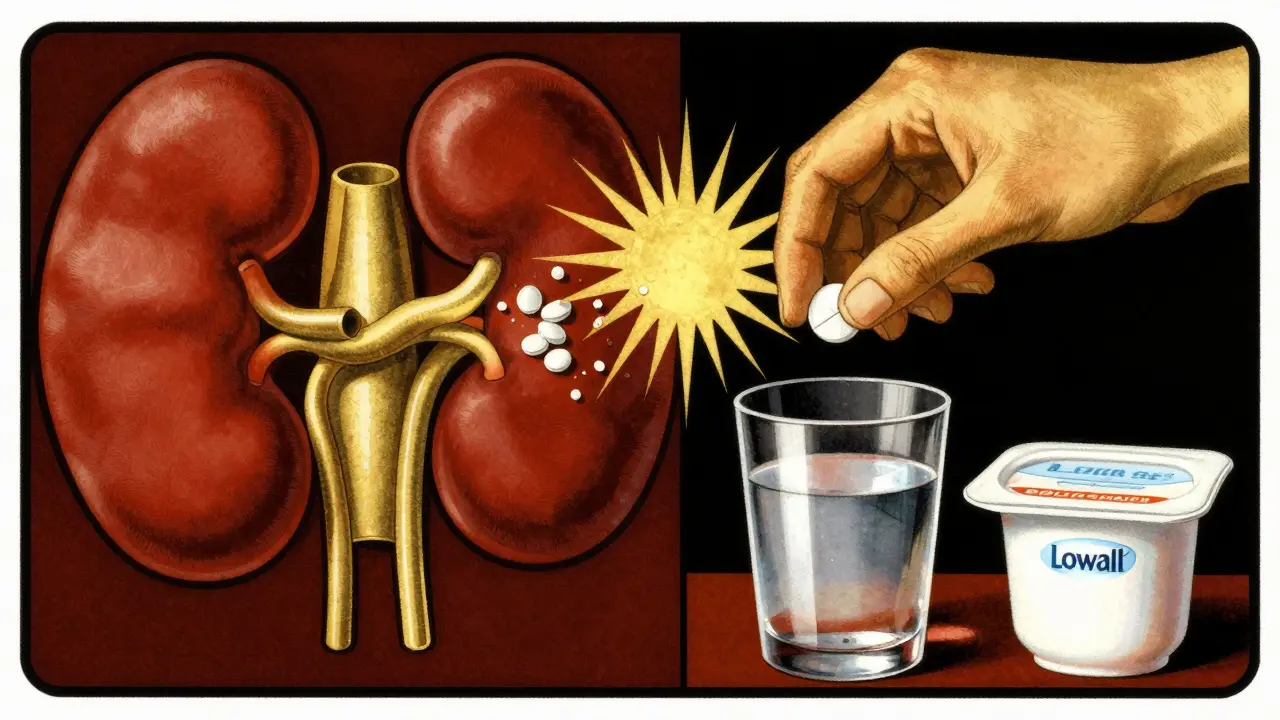
Treating flares is important. But stopping there is like putting a bandage on a leaking pipe. The real goal is to lower your uric acid level enough to prevent crystals from forming at all.The target? Below 6 mg/dL. For people with tophi (those visible lumps of uric acid crystals under the skin), aim for 5 mg/dL or lower. That’s the level where crystals begin to dissolve.
First-line treatment is usually allopurinol. Start low-100 mg daily-and increase by 100 mg every few weeks until your target is reached. Most people need 300-600 mg daily. Some need up to 800 mg. It’s safe for most, even with kidney disease. But rare cases can cause a severe allergic reaction called allopurinol hypersensitivity syndrome. Watch for rash, fever, or worsening kidney function.
If allopurinol doesn’t work or causes side effects, febuxostat (40-80 mg daily) is the next choice. It works similarly but doesn’t need dose adjustments for mild kidney issues. It’s more expensive, though.
Probenecid is a uricosuric drug-it helps your kidneys excrete more uric acid. But it only works if your kidneys are healthy (GFR over 50 mL/min). It’s not for people with kidney stones.
Here’s the critical point: Start urate-lowering therapy with a protective shield. In the first 6 months, you’re very likely to have flares because crystals are dissolving and moving. That’s normal. But you can prevent most of them. Take low-dose colchicine (0.6 mg once or twice daily) during this time. Studies show it cuts flare risk by 50-75%. Skip this step, and you’re setting yourself up for frustration and possibly giving up on treatment.
Diet and Lifestyle That Actually Help
Medication alone isn’t enough. But you don’t need a perfect diet. Small, consistent changes make the difference.- Drink at least 2 liters of water daily. It helps your kidneys flush uric acid.
- Limit beer to less than 12 ounces a day-or better yet, avoid it entirely.
- Swap sugary drinks for water, tea, or coffee. Coffee (regular, not decaf) may even lower your risk slightly.
- Include low-fat dairy-milk, yogurt, cheese. One serving a day reduces gout risk by 43%.
- Choose plant proteins like lentils and tofu over red meat and organ meats.
- Don’t fast or crash diet. Rapid weight loss can spike uric acid.
There’s no magic food that cures gout. But these habits support your treatment and reduce how often you flare.

What Happens If You Stop Taking Your Medication
Many people stop allopurinol or febuxostat when they feel fine. That’s a mistake. Uric acid levels rebound in just 2-4 weeks. Crystals start forming again. Flares return-often worse than before.Gout isn’t cured. It’s managed. Think of it like high blood pressure. You don’t stop your pills because your headache went away. You keep going because the damage is silent until it’s too late.
Regular blood tests every 2-5 weeks during dose adjustments, then every 6 months, are non-negotiable. If your uric acid stays above 6 mg/dL, you’re not doing enough.
New Hope on the Horizon
Research is moving beyond just lowering uric acid. Scientists are now targeting the inflammation itself. Drugs like dapansutrile, which block the NLRP3 inflammasome, are in late-stage trials. Early results show they can cut flare duration by 40%.Another exciting area? The gut microbiome. Early studies suggest certain probiotics may help break down purines in the gut, reducing uric acid by 10-15%. It’s not a replacement for medication yet-but it could become a helpful addition.
For people with long-standing tophi, achieving uric acid levels below 5 mg/dL for a full year leads to complete disappearance of tophi in 70% of cases. That’s not just pain relief. That’s reversing damage.
Final Thoughts: Gout Is Manageable
Gout used to be called the "disease of kings" because it was linked to rich diets and alcohol. Now we know it’s mostly about genetics, kidney function, and lifestyle. It’s not your fault. But it is your responsibility to manage it.You don’t need to give up everything. You don’t need to suffer through every flare. With the right combination of medication, diet, and hydration, you can live without constant pain. The key is consistency. Take your pills. Drink your water. Monitor your levels. And don’t stop just because you feel better. The crystals don’t disappear overnight. But they will-if you give them the chance.
Steven Destiny
December 26, 2025 AT 19:56Finally someone gets it. I used to think gout was just a rich man’s problem until I had my first attack at 32 after one too many beers and a steak dinner. Now I take allopurinol daily, drink water like it’s my job, and avoid sugar like it’s radioactive. It’s not glamorous, but I’d rather walk pain-free than be the guy screaming in the ER again.
Fabio Raphael
December 28, 2025 AT 05:35I’ve been living with this for 8 years. The part about starting urate-lowering meds causing flares? So real. I quit colchicine after 3 months because I thought I was ‘cured.’ Big mistake. Flares came back worse. Started back on it with the low-dose protection plan-life changed. Still hate the diarrhea, but I’d rather have that than the toe-on-fire feeling.
Amy Lesleighter (Wales)
December 30, 2025 AT 04:22uric acid crystals are like tiny glass shards in your joints and your body thinks theyre invaders so it goes full war mode. no wonder it hurts so bad. water water water. and dont stop the pills just cause you feel ok. the crystals dont vanish in a week. theyre patient little bastards.
Becky Baker
December 31, 2025 AT 11:43Why do we even have this disease? We lost the uricase gene? That’s some ancient evolutionary trash. Other animals don’t suffer. We did this to ourselves. Maybe we should’ve kept that gene. This isn’t just a health issue-it’s a national failure.
Natasha Sandra
January 2, 2026 AT 07:32OMG YES 😭 I was so mad when my doc said I needed to give up soda. But then I switched to unsweetened iced tea and my flares dropped by like 70%. Also, low fat yogurt is a secret weapon. I eat it every morning now. You’re not weak for taking meds. You’re smart. 💪❤️
Erwin Asilom
January 3, 2026 AT 02:48Consistency is the only non-negotiable. Medication adherence, hydration, and regular uric acid monitoring are the trifecta. Skipping doses or ignoring lab results is self-sabotage disguised as hope. Gout is not a lifestyle choice-it’s a chronic metabolic condition. Treat it like one.
Sumler Luu
January 4, 2026 AT 18:06I appreciate the detail here. I’ve seen people shame others for drinking wine or eating shrimp. But it’s not about perfection-it’s about patterns. One shrimp platter won’t ruin you. Two a week for five years? That’s the problem. Thank you for not demonizing food.
sakshi nagpal
January 6, 2026 AT 14:07As someone from India where diet is often plant-based, I never thought I’d get gout. But my dad had it, and now I do. The genetics part explained why. I take allopurinol, drink 3 liters of water daily, and avoid beer. Coffee and tofu are my new best friends. It’s manageable if you stay disciplined.
Sandeep Jain
January 6, 2026 AT 23:23i had no idea fructose did this. i thought it was just beer and meat. switched to water and my flares got way better. still take my pill but now i feel like i actually control it. thanks for this
roger dalomba
January 7, 2026 AT 11:24Wow. A medical article that doesn’t sound like it was written by a pharmaceutical rep. Refreshing. Also, yes, the NLRP3 inflammasome is the real villain. Who knew our immune system was this dramatic?
Brittany Fuhs
January 8, 2026 AT 04:23So now we’re blaming evolution? We lost a gene? That’s weak. Real men don’t get gout. You get it because you eat junk, drink like a sailor, and don’t lift weights. Stop making excuses. Just stop being lazy.
Sophia Daniels
January 9, 2026 AT 17:43THEY SAID IT WAS JUST A TOXIN. BUT IT’S WORSE. IT’S A BLOODY REBELLION INSIDE YOUR JOINTS. MACROPHAGES GOING FULL MARINE CORPS ON CRYSTALS LIKE THEY’RE TERRORISTS. COLCHICINE IS THE SILENT SOLDIER. ALLOPURINOL IS THE LONG GAME. AND YOUR WATER BOTTLE? THAT’S YOUR GUN. DON’T YOU DARE PUT IT DOWN.