Illegible Handwriting on Prescriptions: How Poor Writing Puts Patients at Risk and What Actually Works
 Feb, 18 2026
Feb, 18 2026
Imagine this: a doctor writes a prescription. A pharmacist picks it up. They squint. They call back. They guess. And somewhere, a patient gets the wrong dose - or the wrong drug - because a single letter looked like an l but was meant to be a 1. This isn’t a horror movie. It’s real. And it’s happening every day.
Handwritten prescriptions are still around. Not because they’re good. But because they’re stubborn. And the cost? Lives. In the U.S. alone, over 7,000 deaths each year are tied directly to unreadable handwriting on prescriptions, according to the Institute of Medicine. That’s more than plane crashes. More than workplace accidents. And it’s all preventable.
Why Handwritten Prescriptions Are Dangerous
It’s not just about messy penmanship. It’s about what gets missed.
Studies show that 92% of medical students and doctors make at least one prescription error - and most of them are due to unclear writing. Missing initials. Wrong dosages. Confusing "q.d." (once daily) with "q.i.d." (four times daily). A single smudge can turn "500 mg" into "5000 mg". That’s ten times the dose. One mistake. One typo. One life lost.
Pharmacists spend hours on the phone just trying to figure out what was written. In the U.S., they make 150 million calls annually just to clarify prescriptions. Nurses, too. One study found nurses spend an average of 12.7 minutes per illegible prescription trying to track down the right information. That’s over 100 hours a year for each nurse - time that should be spent with patients, not chasing down doctors.
And it’s not just the professionals. Patients suffer too. Delayed treatment. Unnecessary tests. Wrong medications. All because a doctor couldn’t write clearly.
The Numbers Don’t Lie
Here’s what the data says:
- Over 1.5 million preventable adverse drug events happen in the U.S. every year.
- More than 7,000 of those are directly linked to handwriting errors.
- Only 24% of handwritten operative notes were rated as "excellent" or "good" for legibility - 37% were "poor".
- Even among doctors who know the risks, 22% admit they sometimes ignore illegible prescriptions.
And yet, we still let this happen.
E-Prescribing: The Only Real Solution
There’s a fix. And it’s not complicated. It’s called e-prescribing.
Electronic prescriptions don’t rely on handwriting. They use dropdown menus. They auto-fill dosages. They check for drug interactions. They flag allergies. They send the prescription straight to the pharmacy - no phone calls, no guessing.
The results? Stark.
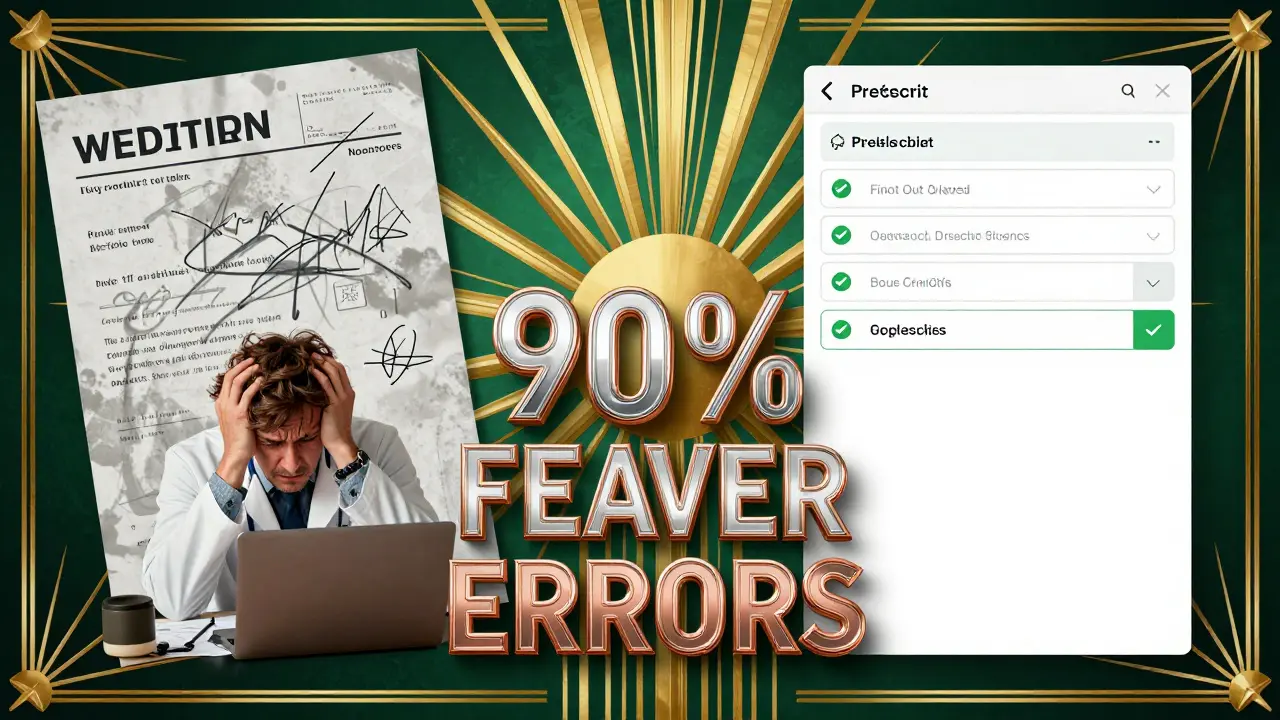
A 2025 study in JMIR compared e-prescriptions to handwritten ones. The accuracy rate? 80.8% for electronic. 8.5% for handwritten. That’s a 90% difference. Nine out of ten errors disappear just by switching to digital.
Even when clinicians manually type in an e-prescription without templates - meaning they still have room for human error - the accuracy rate was still 56%. That’s still six times better than scribbling on paper.
And it’s not just theory. Since 2003, adoption has grown. By 2019, 80% of office-based providers in the U.S. were using e-prescribing. The result? A 97% drop in errors caused by illegible handwriting.
It’s not magic. It’s math.
What’s Holding Us Back?
Some clinics still use paper. Why?
Cost. Training. Legacy systems. Switching to e-prescribing can cost $15,000 to $25,000 per provider. Staff need 8 to 12 hours of training. Integrating with electronic health records takes time. For small clinics, especially in rural or low-resource areas, it’s a big lift.
But here’s the thing: the cost of not switching is higher.
Preventable medical errors cost the U.S. healthcare system an estimated $20 billion a year. That’s not just money. It’s hospital stays. Emergency visits. Lost productivity. Families broken.
And it’s not just about money. It’s about trust. Patients trust that the medicine they’re given is safe. When a pharmacist calls five times to confirm a dose, that trust erodes.
What If You Can’t Go Fully Digital Yet?
Not every clinic has the budget or tech to go fully electronic. But that doesn’t mean you do nothing.
Here’s what works right now:
- Print, don’t write cursive. Block letters are easier to read than loops and swirls.
- Avoid dangerous abbreviations. "U" for units? Could be mistaken for "0" or "cc". "QD"? Could be read as "QID". The Joint Commission has a "Do Not Use" list - use it.
- Write everything. Patient name. Drug name. Exact dose. Route (oral, IV, etc.). Frequency. Prescriber name and contact. No shortcuts.
- Use numbers, not words. Write "5 mg", not "five milligrams". Words are harder to read quickly.
- Double-check. Before signing, pause. Read it like a pharmacist would.
Some clinics have started using checklists. A 2019 study found that when doctors self-assessed their prescriptions using a 15-point checklist, errors dropped significantly. Simple. Low-tech. Effective.
The Future Is Digital - But Not Perfect
E-prescribing isn’t flawless. New problems pop up.
Alert fatigue. Too many pop-ups. Clinicians start ignoring warnings because they’re overwhelmed. Some systems auto-fill the wrong drug because two names sound alike. Others lock you into rigid templates that don’t fit unusual cases.
But these aren’t reasons to go back to paper. They’re reasons to build better systems.
Artificial intelligence is stepping in. Early tools can now interpret handwritten notes with 85-92% accuracy. Imagine a doctor scribbles a script - a camera scans it - and AI cleans it up before it even reaches the pharmacy. It’s not mainstream yet. But it’s coming.
And regulations are pushing it forward. The Medicare Improvements for Patients and Providers Act of 2008 gave financial incentives. The 21st Century Cures Act of 2016 demanded interoperability. Now, the Centers for Medicare & Medicaid Services require meaningful use of electronic records. Paper prescriptions are becoming relics.
What Needs to Happen Next
We need to stop treating illegible handwriting as a "minor" issue. It’s a safety crisis.
Here’s what must change:
- Make e-prescribing mandatory. No exceptions. Not just for hospitals - for every clinic, every private practice.
- Subsidize adoption. Governments and insurers should help small clinics cover the upfront cost. It’s cheaper than paying for the errors.
- Train everyone. Doctors, nurses, pharmacists - all need to understand how e-prescribing reduces risk.
- Design smarter systems. Stop bombarding clinicians with alerts. Build AI that learns from real-world use.
There’s no excuse anymore. We’ve had the tools for over 20 years. We’ve had the proof for decades. The question isn’t whether we can fix this. It’s whether we’re willing to.
What Patients Can Do
You’re not powerless.
- Ask your doctor: "Are you using electronic prescriptions?" If not, ask why.
- Double-check your prescription at the pharmacy. Does the name match what the doctor told you? Is the dose right?
- If something looks off - say something. Don’t assume it’s your mistake.
Medication safety isn’t just the doctor’s job. It’s everyone’s job.
How many deaths are caused by illegible handwriting on prescriptions?
An estimated 7,000 preventable deaths occur each year in the U.S. due to errors caused by unreadable handwriting on prescriptions, according to the Institute of Medicine. These are not accidents - they’re preventable mistakes.
Is e-prescribing really that much safer?
Yes. A 2025 study in JMIR found that electronic prescriptions had an 80.8% accuracy rate for safety compliance. Handwritten prescriptions? Just 8.5%. That’s a 90% drop in errors. Even manually typed e-prescriptions without templates still hit 56% accuracy - far better than paper.
Why do some doctors still write prescriptions by hand?
Cost and habit. Switching to e-prescribing can cost $15,000-$25,000 per provider, plus training time. Some clinics, especially in rural or underfunded areas, can’t afford the upgrade. But the bigger reason? Outdated systems and resistance to change - even though the risks are well documented.
What are the most common errors from bad handwriting?
The top errors include: wrong dosage (like confusing 500 mg with 5000 mg), incorrect frequency (q.d. vs. q.i.d.), wrong drug name (similar-sounding names like "Lanoxin" and "Lanoxin"), and missing route (oral vs. IV). Abbreviations like "U" for units or "QD" are especially dangerous.
Can AI help with handwritten prescriptions?
Yes - but not as a full replacement yet. Early AI tools can interpret handwritten medication names with 85-92% accuracy. This could help clinics still using paper by cleaning up prescriptions before they reach the pharmacy. But AI doesn’t fix poor judgment - it just reduces misreading. The best solution is still full e-prescribing.
What can patients do to protect themselves?
Ask if your doctor uses e-prescribing. Check your prescription label against what your doctor told you. If the dose seems too high or low, ask the pharmacist. Never assume the error is yours - if something feels off, speak up. You’re your own best advocate.