Long-Term Health After Switching to Generic Medications: What Really Happens?
 Nov, 24 2025
Nov, 24 2025
Switching from brand-name drugs to generics is supposed to save money-without sacrificing effectiveness. And for many people, it does. But what happens after six months? Or two years? Or five? The truth is, most studies only check if generics work the same way for a few weeks. That’s not enough when you’re taking a pill every day for decades.
Why the Switch Seems Simple-But Isn’t
The FDA says generics are bioequivalent. That means they deliver the same active ingredient at roughly the same rate and amount as the brand-name version. The acceptable range? Between 80% and 125% of the original drug’s absorption. Sounds tight, right? But that’s a 45% window. One generic could be 80% as strong, another 125%. That’s not a small difference when you’re managing high blood pressure, epilepsy, or heart disease. For some drugs, like statins for cholesterol, switching to generics works great. A 2006 study found people stuck with generic statins 77% of the time-better than the 71% adherence for brand-name versions. And their risk of heart attack or stroke dropped by 8%. That’s the success story everyone talks about. But for others? It’s a different story.When Generics Don’t Stay the Same
A lot of people don’t realize that the same generic drug can come from different manufacturers-even within the same pharmacy. One month you get the pill from Company A, the next from Company B. They’re both FDA-approved. But they look different. Different color. Different shape. Different markings. And that matters. A 2020 University of Pittsburgh study found that 61% of patients felt confused or anxious when their pill changed. One in five reduced how often they took their medicine because they weren’t sure it was the same drug. That’s not just perception-it’s real risk. Missed doses mean worse outcomes. For people with epilepsy, this isn’t theoretical. Pharmacists on Reddit have reported patients who were seizure-free for years on a generic version-until they got switched to a different generic. Seizures returned. Switch back to the original generic? Seizures stopped. Both met FDA bioequivalence standards. But the body didn’t react the same way.The Hidden Cost of Cheap Drugs
It’s easy to assume generics save money. And they do-at the pharmacy counter. But when switching leads to more hospital visits, ER trips, or missed work, the savings vanish. A 2015 review in PharmacoEconomics found that in 64% of cases, total healthcare costs went up after switching to generics. Why? Because patients had more side effects. More complications. More follow-up care. One example: generic antihypertensives. A 2017 Canadian study tracked patients for a year after switching. In the first month, adverse events jumped by 8-14%. And they didn’t drop back down. The patients were still having more dizziness, fatigue, and blood pressure spikes six months later. Even worse, a 2021 study from Ohio State University found that generics made in India had 27% more severe adverse events-including hospitalizations and deaths-than those made in the U.S. The FDA doesn’t track where generics are made on the label. So you might be taking a drug from a factory you’ve never heard of, with no way to know.
Who’s Most at Risk?
Not everyone reacts the same. People with chronic conditions who take meds every day for years are the most vulnerable. That includes:- People with epilepsy or bipolar disorder (narrow therapeutic index drugs)
- Those on blood thinners like warfarin
- Patients with heart failure or kidney disease
- Older adults taking multiple medications
What the Experts Are Saying
Dr. Aaron Kesselheim, a Harvard medical professor, puts it plainly: “The assumption that all generics are interchangeable for all patients over the long term isn’t supported by evidence.” Dr. Jerry Avorn, also from Harvard, adds: “The 80-125% range allows for clinically meaningful differences-especially after years of daily use.” Even the American College of Physicians warns: Don’t switch patients multiple times between different generic manufacturers, especially for critical drugs. One switch might be fine. Two or three? That’s when trouble starts. And then there’s Dr. Corey Nislow from the University of British Columbia. His team found DNA-damaging contaminants in nearly 4 out of 10 generic drugs tested. These aren’t acute poisons. They’re slow, silent threats-possibly linked to long-term organ damage or cancer risk. But we don’t have data yet because no one’s been tracking it.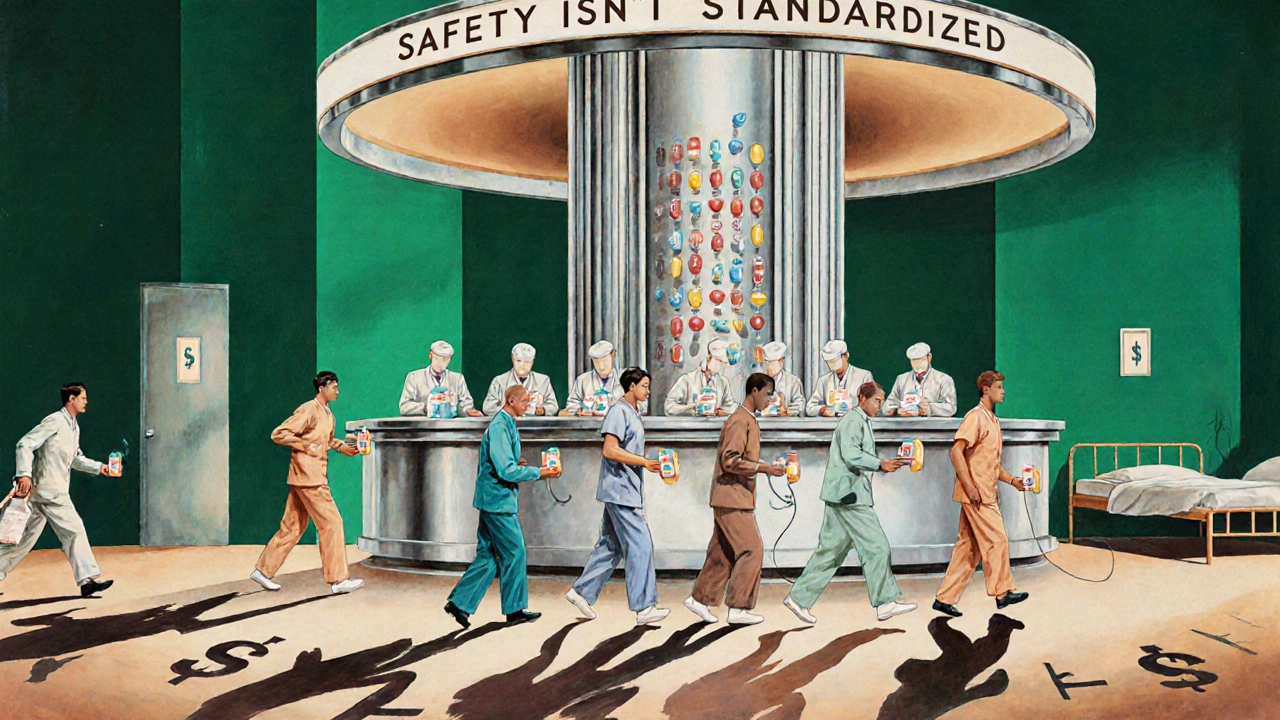
How to Protect Your Health After Switching
You don’t have to avoid generics. But you do need to be smart about it. Here’s what actually works:- Ask your doctor to write “Dispense as Written” or “Do Not Substitute” on your prescription-especially for epilepsy, blood thinners, or heart meds. Pharmacists can’t switch it without your doctor’s OK.
- Know your pill. Take a photo of your medication when you get it. Note the color, shape, and imprint. If it changes next refill, ask why.
- Stick with one manufacturer. If you find a generic that works, ask your pharmacist to keep ordering it. Don’t let them swap it out.
- Track your symptoms. Keep a simple log: energy levels, mood, side effects, any new symptoms. Share it with your doctor at every visit.
- Don’t panic if you switch-but monitor closely. If you feel worse in the first 30-60 days, don’t assume it’s “all in your head.” Go back to your doctor. Ask if it could be the new generic.
What’s Changing-And What’s Not
The FDA is finally starting to wake up. In 2023, they began requiring 36 months of stability data for generics used in chronic conditions. That’s a big step. Previously, most data only covered 24 months. In Europe, countries like Germany and France now require 24 months of real-world safety data before allowing automatic substitution for critical drugs. But here’s the problem: most U.S. health systems still don’t track which generic manufacturer you’re on. Only 35% of electronic health records even record it. So if you switch doctors or pharmacies, your history vanishes. Meanwhile, pharmacy benefit managers (PBMs)-the middlemen who control which drugs are covered-still force automatic switches. Nearly 70% of Medicare Part D plans change their preferred generics every year. That’s not patient care. That’s cost-cutting.Bottom Line: Generics Are a Tool, Not a Guarantee
Generics saved the U.S. healthcare system over $1.6 trillion between 2008 and 2017. That’s real progress. For millions, they make life-saving drugs affordable. But affordability shouldn’t come at the cost of long-term safety. If you’re on a generic drug for a chronic condition, you have the right to know:- Which manufacturer made your pill
- Whether it’s been switched recently
- What side effects to watch for
- How to tell if it’s still working
Pallab Dasgupta
November 26, 2025 AT 01:57Bro, I switched my blood pressure med to generic last year and felt like a zombie for three months-dizzy, sluggish, zero motivation. Thought it was depression. Turns out, my pharmacy swapped the manufacturer twice without telling me. Now I demand the same brand every time. My doctor wrote ‘Do Not Substitute’ on my script. Worth the extra $5.
Also, why the hell does the FDA not track where these pills come from? I’m not taking some mystery powder from a factory in Gujarat that my pharmacist can’t even name.
Amy Hutchinson
November 27, 2025 AT 17:11OMG I’m so glad someone finally said this. My mom’s on warfarin and they switched her generic and she almost had a stroke. Like, she was fine for years, then BAM-bruising everywhere, nosebleeds, panic attacks. They didn’t even call to warn her. This isn’t science, it’s a lottery.
Archana Jha
November 29, 2025 AT 09:20Wait wait wait-so you’re telling me the FDA lets companies make pills that can be 45% weaker OR stronger and calls it ‘safe’? And we’re supposed to trust this? Lol. I think Big Pharma and the FDA are in cahoots with the Indian manufacturing mafia. Remember the baby formula scandal? Same playbook. They don’t care if you die slowly from organ failure as long as the stock price goes up. Also, did you know glyphosate is in 70% of generics? I read it on a blog. It’s in the coating. It’s a slow poison. They’re testing it on us.
Aki Jones
November 30, 2025 AT 15:02It’s not merely a bioequivalence issue-it’s a systemic failure of pharmacovigilance infrastructure. The 80–125% confidence interval, while statistically permissible, is clinically indefensible for drugs with narrow therapeutic indices. Moreover, the absence of longitudinal adverse event tracking in electronic health records-coupled with PBM-driven formulary churn-constitutes a violation of the duty of care. The FDA’s 2023 stability requirement is a performative gesture; without mandatory manufacturer labeling and patient-level longitudinal registries, this remains a regulatory charade.
Jefriady Dahri
November 30, 2025 AT 21:03Hey, I get it. I’m from India, and I’ve seen how these meds are made. But don’t throw the baby out with the bathwater. My cousin in Delhi takes a generic for epilepsy and hasn’t had a seizure in 8 years. The problem isn’t generics-it’s the flip-flopping. Stick with one brand. Know your pill. Take a pic. Talk to your pharmacist. It’s not hard.
And yes, some Indian factories are sketchy-but so are some U.S. ones. I’ve seen U.S.-made generics with mold in the bottle. It’s about accountability, not geography. Be smart, not scared. 💪
Erika Hunt
December 1, 2025 AT 06:38I think this whole conversation needs to be reframed-not as ‘generics are bad’ or ‘brand names are better,’ but as ‘we need more transparency and consistency in medication supply chains.’ The fact that patients are being switched without notification, without documentation, and without follow-up is the real issue. The FDA’s job isn’t just to approve drugs-it’s to ensure that the system doesn’t accidentally harm people who are already vulnerable. And right now, it’s failing. We need a universal pill identifier, mandatory manufacturer tracking in EHRs, and mandatory patient education when a switch occurs. It’s not rocket science. It’s basic patient safety.
Roscoe Howard
December 1, 2025 AT 20:10It is, indeed, an unfortunate circumstance that the United States has permitted the importation of pharmaceuticals from jurisdictions with suboptimal regulatory oversight. The integrity of the American healthcare system is being undermined by the commodification of life-saving medications. One must ask: why should an American citizen be subjected to the pharmacological whims of foreign manufacturers with lax quality controls? The solution is simple: ban the importation of generics from nations that do not meet U.S. GMP standards. Period.
Ellen Sales
December 2, 2025 AT 19:41My dad’s been on the same generic statin for 12 years. Same pill. Same color. Same imprint. He’s 78, runs 5Ks, and his cholesterol’s perfect. He didn’t even know there was a difference between generics until I showed him this post.
Here’s the truth: if you’re stable, don’t touch it. If you’re not stable, don’t let them switch you. And if you’re confused? You’re not crazy. You’re paying attention.
This isn’t about being anti-generic. It’s about being pro-stability. Pro-consistency. Pro-owning your own health. You’re not a data point. You’re a person. And your body remembers what it’s been given.
Take the photo. Write it down. Ask for the name on the bottle. That’s your power.
Josh Zubkoff
December 4, 2025 AT 19:28Okay, so let me get this straight: the FDA approves drugs based on a 45% absorption window, pharmacies swap pills like baseball cards, patients get confused, side effects spike, and then the system says ‘it’s fine because the math adds up’? This isn’t healthcare. This is a horror movie where the villain is a spreadsheet. And the worst part? We’re all just supposed to shrug and say ‘well, it’s cheaper.’
Meanwhile, the CEO of the PBM who forced that switch just bought a private island. And you’re telling me the person on the other end of that pill bottle is just supposed to ‘monitor symptoms’? Like it’s a TikTok challenge? ‘Day 37: Still dizzy. Still tired. Still alive. #GenericStruggles.’
This isn’t a medical issue. It’s a moral failure.
fiona collins
December 4, 2025 AT 23:52My pharmacist always tells me the manufacturer name when I pick up my prescription. It takes 10 seconds. Why doesn’t everyone do that?