Skin Rashes and Medication-Induced Dermatitis: What Patients Should Know
 Nov, 20 2025
Nov, 20 2025
Drug Rash Risk Assessment Tool
When you start a new medication, you expect it to help - not hurt. But for some people, the very drug meant to treat one problem ends up causing another: a skin rash. It might start as a few red spots, then spread. It itches. It burns. Sometimes, it blisters. And if you don’t recognize it for what it is, you could be at risk for something far more serious.
What Exactly Is a Drug-Induced Rash?
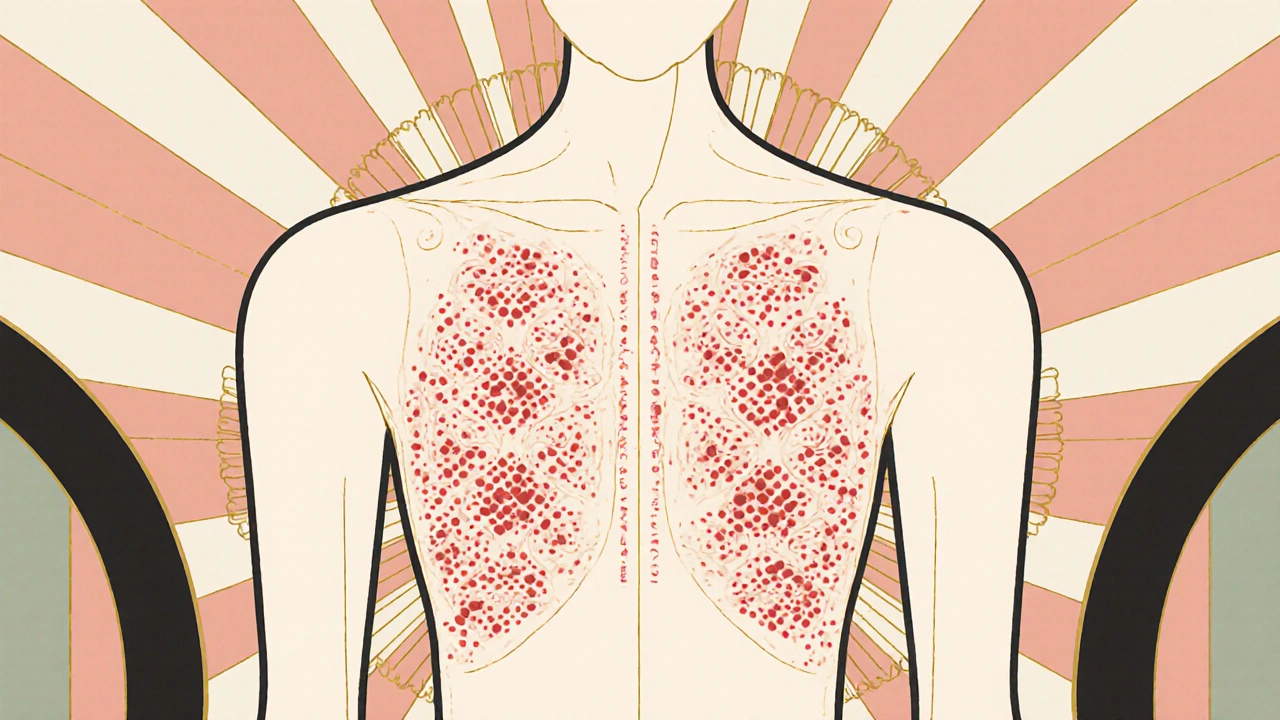
A drug-induced rash, or medication-induced dermatitis, is a skin reaction caused by a medicine. It’s not rare. About 2 to 5% of all adverse drug reactions show up on the skin. That means if you’re taking even one prescription, you’re not immune. The most common type is a morbilliform rash - red, flat spots or small bumps that look like measles. It usually shows up 4 to 14 days after starting the drug, often starting on the chest or back and spreading outward.
But not all drug rashes are the same. Some are allergic. Others aren’t. And knowing the difference can save your life.
Common Types of Drug Rashes and How They Look
There are several patterns doctors look for. The most frequent - making up 60 to 70% of cases - is the morbilliform rash. It’s usually mild. It itches, but doesn’t blister. And if you stop the medicine, it clears up in 1 to 2 weeks.
Then there’s drug-induced urticaria - hives. These are raised, red, itchy welts that come and go. They can appear within minutes of taking a pill. If they’re the only symptom, they’re usually not dangerous. But if they’re paired with swelling of the lips, tongue, or throat, or trouble breathing, that’s an emergency.
DRESS syndrome is less common but far more serious. It doesn’t just hit the skin. It affects your liver, kidneys, lungs, or blood. You might get a fever, swollen glands, and a widespread rash that looks like a bad sunburn. It usually shows up 2 to 6 weeks after starting the drug. The biggest culprits? Antiseizure meds like carbamazepine, phenytoin, and lamotrigine. Allopurinol (used for gout) and certain antibiotics like sulfonamides are also high-risk. About 1 in every 1,000 to 10,000 people who take these drugs will develop DRESS. And if you don’t get treated, it can be fatal.
Stevens-Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TEN) are the most dangerous. The skin starts to blister and peel off, like a severe burn. Mucous membranes - your mouth, eyes, genitals - can also be damaged. SJS has a 5 to 15% death rate. TEN? Up to 35%. These reactions usually happen within the first 8 weeks of taking the drug. Medications linked to them include antibiotics (especially penicillin), NSAIDs like ibuprofen, anticonvulsants, and allopurinol.
Then there’s nummular dermatitis. These are coin-shaped, red, scaly patches. They can be mistaken for eczema. But if they appear after starting a new drug - and clear up fast after stopping it - that’s a clue. Drug-induced nummular dermatitis heals in 4 to 8 weeks. The non-drug kind? Could last years.
What Medications Cause the Most Rashes?
Some drugs are far more likely to trigger skin reactions than others. Penicillin and related antibiotics cause about 10% of all drug rashes. Sulfa drugs (like Bactrim) are next. Antiseizure medications - carbamazepine, phenytoin, lamotrigine - are notorious for causing severe reactions, especially in people with certain genetic markers. Allopurinol, used for gout, is another major offender.
Even common over-the-counter meds can be the culprit. NSAIDs like ibuprofen and naproxen cause non-allergic rashes in about 25% of cases. They don’t involve the immune system - they just irritate the skin directly. Tetracycline antibiotics, especially doxycycline, and fluoroquinolones like ciprofloxacin can cause photosensitivity. You get a rash only where the sun hits your skin - neck, arms, shoulders.
Chemotherapy drugs? High risk. Diuretics like hydrochlorothiazide? Also linked to sun-triggered rashes. And if you’re on multiple meds - five or more - your chance of developing a drug rash jumps to 35%. For someone taking just one or two? Only 5%.

Why Some People React and Others Don’t
It’s not random. Genetics play a big role. People of Southeast Asian descent who carry the HLA-B*1502 gene are 1,000 times more likely to develop SJS from carbamazepine. Han Chinese with the HLA-B*5801 gene have a 580-fold higher risk of a deadly reaction to allopurinol. That’s why some doctors test for these genes before prescribing.
Other factors? Viral infections. If you have Epstein-Barr virus (mononucleosis) or HIV and take an antibiotic like amoxicillin, your chance of a rash skyrockets - up to 10 times higher. People with weakened immune systems - from cancer, transplants, or autoimmune disease - are also more vulnerable.
And here’s something many don’t realize: you can become allergic to a drug after your first exposure. Your immune system doesn’t always react right away. It might take a second or third time taking it before it recognizes the drug as a threat. That’s why you might have taken penicillin before with no problem - then suddenly break out in hives on the third round.
What to Do If You Get a Rash
Don’t panic. But don’t ignore it either.
Stop the medication? Only if your doctor says so. Never quit a drug like an antiseizure medicine or blood pressure pill on your own. Stopping suddenly can be deadly.
Call your doctor immediately if you have:
- Blisters or peeling skin
- Sores in your mouth, eyes, or genitals
- Fever, swollen lymph nodes, or joint pain
- Difficulty breathing or swelling of the face, lips, or tongue
These are red flags for SJS, DRESS, or anaphylaxis. Go to the ER. Don’t wait.
For mild rashes - just red, itchy spots with no other symptoms - your doctor might suggest:
- Lukewarm baths with gentle, soap-free cleansers
- Applying fragrance-free moisturizer within 3 minutes of bathing
- Over-the-counter hydrocortisone cream (1%) twice a day
For more severe cases, you might need a stronger steroid cream like clobetasol, or even oral prednisone.

How Doctors Diagnose Drug Rashes
There’s no single test. Diagnosis is mostly detective work. Your doctor will ask:
- When did you start the medication?
- What else are you taking? (Including supplements and OTC drugs)
- Have you had this rash before?
- Are you sick with a virus right now?
They’ll look at the rash pattern. The timing. Your medical history. Sometimes, they’ll do a skin biopsy. Or a patch test. For penicillin allergies, skin testing is now 95% accurate - so if you think you’re allergic, get tested. About 15% of people who say they’re allergic to penicillin aren’t. They just had a rash years ago. Avoiding penicillin unnecessarily means you get stronger, costlier antibiotics - which can lead to worse infections down the road.
How to Prevent Future Reactions
Once you know what caused your rash, keep a record. Write down the drug name, the type of rash, and when it happened. Share this with every doctor you see.
Ask: “Could this drug cause a skin reaction?” Especially if you’re starting something new. If you have a known allergy, wear a medical alert bracelet.
And if you’re over 65 or taking five or more medications? Be extra careful. Polypharmacy is the biggest risk factor for drug rashes today. Your body doesn’t process drugs the same way it did when you were younger. What was safe at 30 might be dangerous at 70.
The Bottom Line
Most drug rashes are harmless and go away once you stop the medicine. But a small number - less than 2% - are life-threatening. The key is knowing the signs and acting fast.
If you get a rash after starting a new drug, don’t assume it’s just a coincidence. Don’t wait to see if it gets worse. Talk to your doctor. Get it checked. And remember: the goal isn’t to avoid all medications. It’s to use them safely. You don’t have to live in fear. You just need to be informed.
Noah Fitzsimmons
November 20, 2025 AT 10:29Eliza Oakes
November 21, 2025 AT 13:19Simone Wood
November 22, 2025 AT 19:21Sammy Williams
November 24, 2025 AT 16:00Steve Harris
November 26, 2025 AT 13:02Michael Marrale
November 27, 2025 AT 12:10David vaughan
November 28, 2025 AT 17:15Cooper Long
November 29, 2025 AT 22:14Sheldon Bazinga
November 30, 2025 AT 10:13Sandi Moon
November 30, 2025 AT 23:56Kartik Singhal
December 1, 2025 AT 19:37Logan Romine
December 2, 2025 AT 16:33Chris Vere
December 4, 2025 AT 08:46Pravin Manani
December 5, 2025 AT 20:38