Systemic Antifungals and Dangerous Interactions with Statins & Immunosuppressants
 Oct, 26 2025
Oct, 26 2025
Antifungal-Statins-Immunosuppressants Interaction Checker
Check Interaction Risk
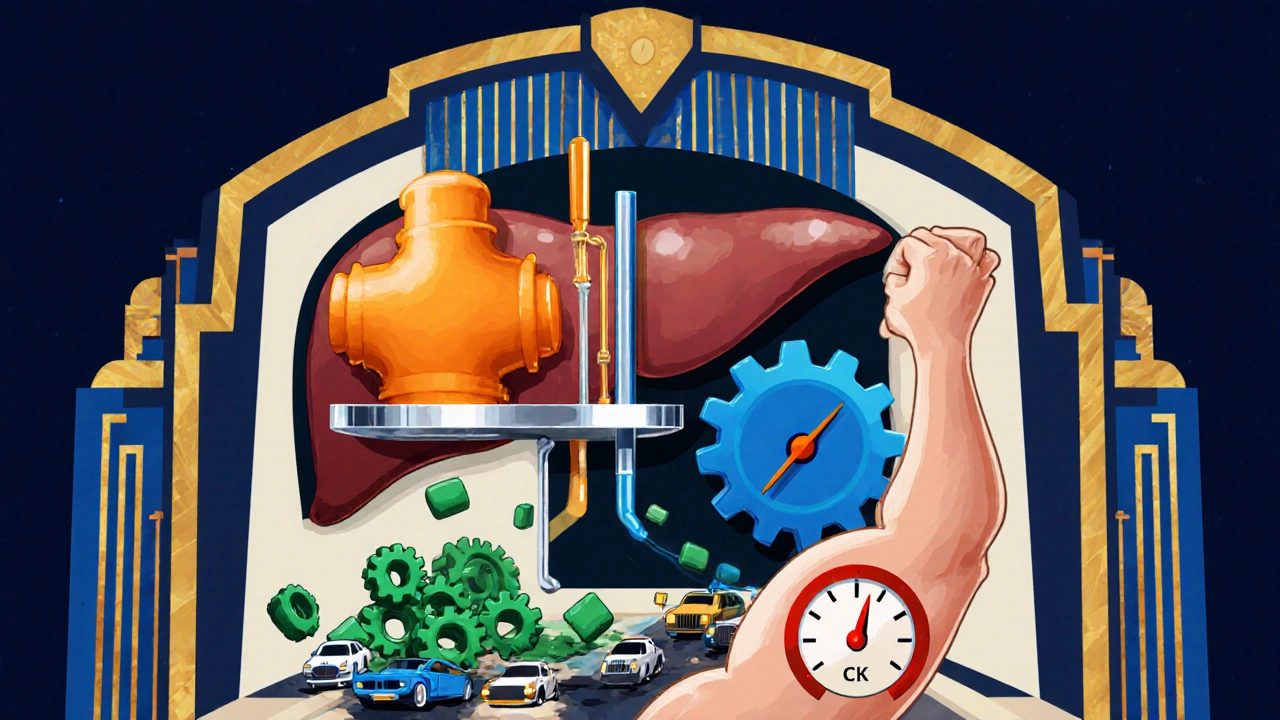
Patients on cholesterol‑lowering pills or transplant meds often hear a warning about mixing them with certain antifungal drugs. The reality is that many systemic antifungals slam the brakes on the same liver enzymes that clear statins and immunosuppressants, turning a routine prescription into a potential medical emergency. Below you’ll find exactly how those interactions happen, which drug combos are most hazardous, and what steps clinicians can take to keep patients safe.
How systemic antifungals work - the azole connection
Systemic Antifungal is a medication that treats invasive fungal infections by targeting the fungal cell membrane. Most of these drugs belong to the azole class, which blocks the enzyme lanosterol 14‑α‑demethylase, a cytochrome P450 (CYP) enzyme essential for converting lanosterol to ergosterol. Without ergosterol, the fungal membrane becomes leaky and the organism dies (StatPearls, 2023).
Azoles are divided into two families. The older imidazoles (ketoconazole, clotrimazole, miconazole) and the newer triazoles (itraconazole, voriconazole, posaconazole, fluconazole). While triazoles tend to have a better safety profile, they all share a knack for inhibiting human CYP enzymes, especially CYP3A4, and drug transporters like P‑glycoprotein (P‑GP) and OATP1B1.
Statins - why they’re vulnerable
Statin is a class of drugs that lowers LDL cholesterol by blocking HMG‑CoA reductase. Many statins - atorvastatin, simvastatin, lovastatin - are metabolized primarily by CYP3A4. When a strong CYP3A4 inhibitor is added, the statin’s blood level can spike ten‑fold, dramatically raising the odds of statin‑associated myopathy (SAM) and, in severe cases, rhabdomyolysis.
Pravastatin and rosuvastatin rely less on CYP metabolism, but they still depend on transporters such as OATP1B1. Inhibiting those transporters (as ketoconazole does) can also lift their concentrations, albeit to a lesser degree.
Immunosuppressants - the double‑hit problem
Immunosuppressant is a drug used to prevent organ rejection or to treat autoimmune conditions. Key agents - cyclosporine, tacrolimus, sirolimus, everolimus - are themselves CYP3A4 substrates and often inhibit the same enzyme and transporters. When a patient takes both an immunosuppressant and a statin, the two drugs compete for the same metabolic pathways, pushing statin exposure even higher.
Studies in solid‑organ transplant recipients show that statin AUC can increase 3‑ to 20‑fold when paired with cyclosporine, leading to myalgia in up to 25 % of patients and rhabdomyolysis in a small but deadly fraction.
Azole agents and their CYP inhibition strength
The interaction risk hinges on how potently each azole blocks CYP enzymes. Below is a quick reference:
| Azole | CYP3A4 | CYP2C19 | CYP2C9 | Transporter Effect |
|---|---|---|---|---|
| Ketoconazole | Strong inhibitor | Weak | Weak | Inhibits OATP1B1 & P‑GP |
| Itraconazole | Potent inhibitor (substrate) | Moderate | Weak | Minor transporter impact |
| Voriconazole | Potent | Moderate | Weak | Minimal |
| Posaconazole | Strong | Weak | Negligible | Inhibits OATP1B1 |
| Fluconazole | Moderate | Strong | Moderate | Minimal |
Notice that ketoconazole and posaconazole sit at the top of the risk ladder for statin interactions because they combine strong CYP3A4 inhibition with transporter blockage.
Clinical consequences of high‑risk combos
When statin levels surge, the most common manifestation is muscle pain (myalgia). If unchecked, muscle breakdown releases creatine kinase (CK) into the bloodstream. CK values above 10 000 U/L are a red flag for rhabdomyolysis, which can cause acute kidney injury and, in rare cases, death.
Case reports describe transplant patients on cyclosporine and a 10 mg dose of simvastatin who developed CK spikes of 15 000 U/L within days of adding ketoconazole. The same pattern appears with azole‑statin combos: a patient on atorvastatin (40 mg) and posaconazole for invasive aspergillosis suffered severe myopathy after just two weeks, requiring statin discontinuation and aggressive hydration.

Management strategies - what clinicians should do
Preventing these events is a matter of proactive drug‑selection, dose‑adjustment, and monitoring. Below is a step‑by‑step protocol that can be baked into pharmacy verification or electronic health record alerts.
- Identify the azole and the statin (or immunosuppressant) before the prescription is written.
- If the azole is a strong CYP3A4 inhibitor (ketoconazole, itraconazole, posaconazole), hold atorvastatin, simvastatin, and lovastatin for the duration of antifungal therapy.
- If a statin must be continued, switch to pravastatin (10‑40 mg) or rosuvastatin (5‑20 mg) at the lowest effective dose.
- For patients on immunosuppressants, reduce the statin dose by at least 50 % and check trough levels of the immunosuppressant after starting or stopping the azole.
- Monitor CK and renal function at baseline, then weekly for the first two weeks of combined therapy, then monthly if stable.
- Educate patients to report any unexplained muscle pain, weakness, or dark urine immediately.
Therapeutic drug monitoring (TDM) of tacrolimus or cyclosporine is especially important because azoles can raise their concentrations 30‑50 % and increase nephrotoxicity risk.
Practical checklist for prescribers and pharmacists
- Is the antifungal an azole? Check the inhibition table above.
- Is the statin a CYP3A4 substrate? (atorvastatin, simvastatin, lovastatin)
- Is the patient on an immunosuppressant that also uses CYP3A4?
- Choose alternative statin (pravastatin/rosuvastatin) or hold the statin.
- Adjust immunosuppressant dose and order TDM.
- Document CK baseline; repeat if muscle symptoms appear.
- Set up electronic alerts for high‑risk combos.
Institutions that have embedded such checklists into their pharmacy workflow report up to a 63 % drop in dangerous azole‑statin pairings.
Future directions - safer antifungals and personalized risk
Newer agents like isavuconazole offer moderate CYP3A4 inhibition, reducing interaction severity compared with older azoles. Even more promising is olorofim, which works through dihydroorotate dehydrogenase inhibition and shows negligible CYP involvement in early trials - a potential game‑changer for patients who need both antifungal and lipid‑lowering therapy.
Pharmacogenomics is also entering the scene. About 12 % of people carry SLCO1B1 variants that impair OATP1B1 function, making them inherently prone to statin myopathy. When such a patient receives a CYP3A4 inhibitor, the combined effect can be catastrophic. Routine genotyping could let clinicians pre‑emptively avoid high‑risk combos.
Which statins are safest to use with azole antifungals?
Pravastatin and rosuvastatin have the lowest CYP3A4 metabolism and are least affected by azole‑induced enzyme inhibition. Dose reductions (e.g., pravastatin 10‑20 mg) are usually sufficient, but clinicians should still watch CK levels.
Do all azoles require stopping statins?
Strong inhibitors such as ketoconazole, itraconazole, and posaconazole generally demand that CYP3A4‑metabolized statins be held. Moderate inhibitors like fluconazole may allow dose reductions rather than full discontinuation, but close monitoring is still advised.
How often should CK be checked when patients are on both drugs?
Baseline CK before starting the combination, then weekly for the first two weeks, followed by monthly checks if no symptoms arise. Immediate testing is needed at any sign of muscle pain.
Can therapeutic drug monitoring help with immunosuppressants?
Yes. Because azoles raise cyclosporine and tacrolimus levels, TDM should be performed 3‑5 days after any change in antifungal therapy, with dose adjustments made to keep trough concentrations in target ranges.
Are there any non‑azole antifungals that avoid these interactions?
Echinocandins (caspofungin, micafungin, anidulafungin) and the newer agent olorofim have minimal CYP involvement, making them safer choices when concurrent statin or immunosuppressant therapy is essential.
Alisha Cervone
October 26, 2025 AT 15:30Interesting read
Ben Dover
November 1, 2025 AT 10:23The pharmacokinetic interplay delineated herein warrants meticulous scrutiny; systemic azoles, particularly ketoconazole, possess a formidable inhibitory capacity against CYP3A4, thereby engendering supra‑therapeutic statin concentrations. One must appreciate the quantitative magnitude of such interactions, as evidenced by documented ten‑fold elevations in atorvastatin AUC. Consequently, the risk of myopathy escalates commensurately, rendering routine co‑prescription perilous without dose adjustments. It is incumbent upon clinicians to incorporate therapeutic drug monitoring and CK surveillance as standard protocol. Moreover, the delineated checklist offers a pragmatic framework for mitigating iatrogenic harm.
Katherine Brown
November 7, 2025 AT 05:16While the mechanistic exposition is comprehensive, it is essential to recognize the heterogeneity among patients regarding genetic polymorphisms that affect transporter function. The inclusion of SLCO1B1 genotyping could further refine risk stratification. In practice, a collaborative approach between pharmacy and infectious disease services optimizes patient safety. Hence, the recommendations merit integration into institutional protocols.
Tony Stolfa
November 13, 2025 AT 00:10Yo, if you’re gonna mash up azoles with statins, expect a freakin’ explosion in drug levels. No one wants to be on the floor with rhabdo, so just ditch the statin while you’re on the strong azole.
Joy Dua
November 18, 2025 AT 19:03The ontological ramifications of pharmacodynamic synergy cannot be dismissed; the azole‑statin axis epitomizes a paradox wherein therapeutic intent begets toxicity. By interrogating the enzymatic cascade one discerns a deterministic pattern wherein CYP3A4 inhibition precipitates an inexorable rise in statin plasma concentration. It follows that preemptive cessation of atorvastatin is not merely advisable but ethically mandated. Such a stance aligns with the principle of non‑maleficence. Nevertheless, the discourse must also consider patient adherence challenges inherent to regimen alteration.
Holly Kress
November 24, 2025 AT 13:56Great synthesis of the literature. I appreciate the practical checklist; it makes implementation much easier. Let’s keep the focus on patient education and monitoring.
Chris L
November 30, 2025 AT 08:50Absolutely, the checklist is a solid starting point. In my experience, involving the patient early on improves compliance with CK monitoring. Adjusting doses collaboratively also reduces the chance of adverse events. Together we can ensure safety without compromising antifungal efficacy.
Charlene Gabriel
December 6, 2025 AT 03:43When contemplating the concurrent administration of systemic azole antifungals and lipid‑lowering agents, several pivotal considerations emerge that extend beyond the mere biochemical inhibition of cytochrome P450 isoforms. First, the clinician must evaluate the baseline risk profile of the patient, including existing hepatic or renal impairment, which can amplify the pharmacokinetic perturbations induced by CYP3A4 blockade. Second, the selection of a statin with minimal reliance on CYP3A4 metabolism, such as pravastatin or rosuvastatin, can markedly attenuate the magnitude of drug‑drug interaction, yet this substitution is not universally sufficient; transporter inhibition by agents like ketoconazole may still elevate statin concentrations. Third, therapeutic drug monitoring of immunosuppressants such as tacrolimus and cyclosporine becomes indispensable, as azole‑mediated inhibition can precipitate a 30‑50 % increase in trough levels, potentially leading to nephrotoxicity. Fourth, a structured schedule for creatine kinase (CK) assessment should be instituted-baseline measurement followed by weekly checks during the initial two weeks of combined therapy, transitioning to monthly surveillance if the patient remains asymptomatic. Fifth, patients should receive clear, jargon‑free education regarding the early signs of myopathy, including unexplained muscle soreness, weakness, or dark‑colored urine, and be instructed to report these symptoms immediately. Sixth, electronic health record (EHR) alerts can serve as a safety net, flagging high‑risk drug‑pairings and prompting prescribers to consider dose adjustments or alternative agents. Seventh, the emerging class of non‑azole antifungals, such as echinocandins and the novel agent olorofim, offers a viable therapeutic avenue with negligible CYP interaction potential, thereby circumventing the need for complex dose modifications altogether. Eighth, pharmacogenomic profiling, particularly for SLCO1B1 variants, holds promise for preemptively identifying individuals at heightened risk for statin‑induced myopathy, allowing for personalized medication selection. Ninth, interdisciplinary collaboration between infectious disease specialists, pharmacists, and transplant teams ensures a cohesive approach to balancing antifungal efficacy with cardiovascular risk mitigation. Tenth, documentation of all interventions, dose changes, and monitoring results is critical for continuity of care and medico‑legal protection. Eleventh, when possible, a short course of high‑intensity statin therapy should be avoided in favor of moderate‑intensity agents to reduce the exposure window. Twelfth, dose‑adjustment algorithms, such as halving the atorvastatin dose when co‑prescribed with a strong CYP3A4 inhibitor, provide a pragmatic compromise when statin continuation is unavoidable. Thirteenth, institutions that have integrated these multifaceted strategies into their antimicrobial stewardship programs report reductions in adverse events exceeding 60 %. Fourteenth, ongoing education and case reviews reinforce best practices and keep the clinical team apprised of evolving guidelines. Fifteenth, ultimately, the goal is to harmonize the dual imperatives of eradicating invasive fungal infections while safeguarding cardiovascular health, a balance achievable through diligent assessment, vigilant monitoring, and proactive communication.
Leah Ackerson
December 11, 2025 AT 22:36Whoa, this stuff is like a hidden trap for the unsuspecting 🤔💊. If you don’t watch those statins, you could end up with muscles that feel like they’re on fire 🔥. Always keep an eye on CK levels, or you might be in for a painful surprise 😬.
Gary Campbell
December 17, 2025 AT 17:30What they don’t tell you is that the pharmaceutical giants are hiding the true extent of these interactions to keep you on their drugs longer. The data shows a pattern of suppressed adverse event reporting. It’s no coincidence that the same companies own the labs that test for CK levels. Stay skeptical and demand full transparency.
renee granados
December 23, 2025 AT 12:23Do not trust the warnings. They are made up. Check your own health. If you feel pain stop the meds.
Stephen Lenzovich
December 29, 2025 AT 07:16This is a classic case of foreign influence on our medical guidelines. We must protect our patients from unnecessary restrictions. The real solution is to keep using the strongest statins no matter what they say. Our health system should prioritize American pharmaceutical independence.
abidemi adekitan
January 4, 2026 AT 02:10Thank you for the thorough overview. I’ll share this with my team and we’ll incorporate the checklist into our daily rounds. Collaborative vigilance is key.
Barbara Ventura
January 9, 2026 AT 21:03Wow, what a detailed piece, truly enlightening, and incredibly useful, especially for those of us who juggle multiple prescriptions, and need clear guidance, every single time, it’s a lifesaver.
laura balfour
January 15, 2026 AT 15:56I must say, the way this article breaks down the complex world of drug interactions is simply superb! It reads like a masterclass, yet the occasional typo-like "interacctions"-makes it feel more human. Still, the depth of analysis is commendable and will definitely help many clinicians navigate these tricky waters.