Understanding Adverse Event Rates: Percentages and Relative Risk in Clinical Trials
 Jan, 27 2026
Jan, 27 2026
Adverse Event Rate Calculator
Compare IR vs. EAIR for Your Trial Data
Enter data for two trial groups to see how Incidence Rate (IR) and Exposure-Adjusted Incidence Rate (EAIR) differ when treatment durations vary.
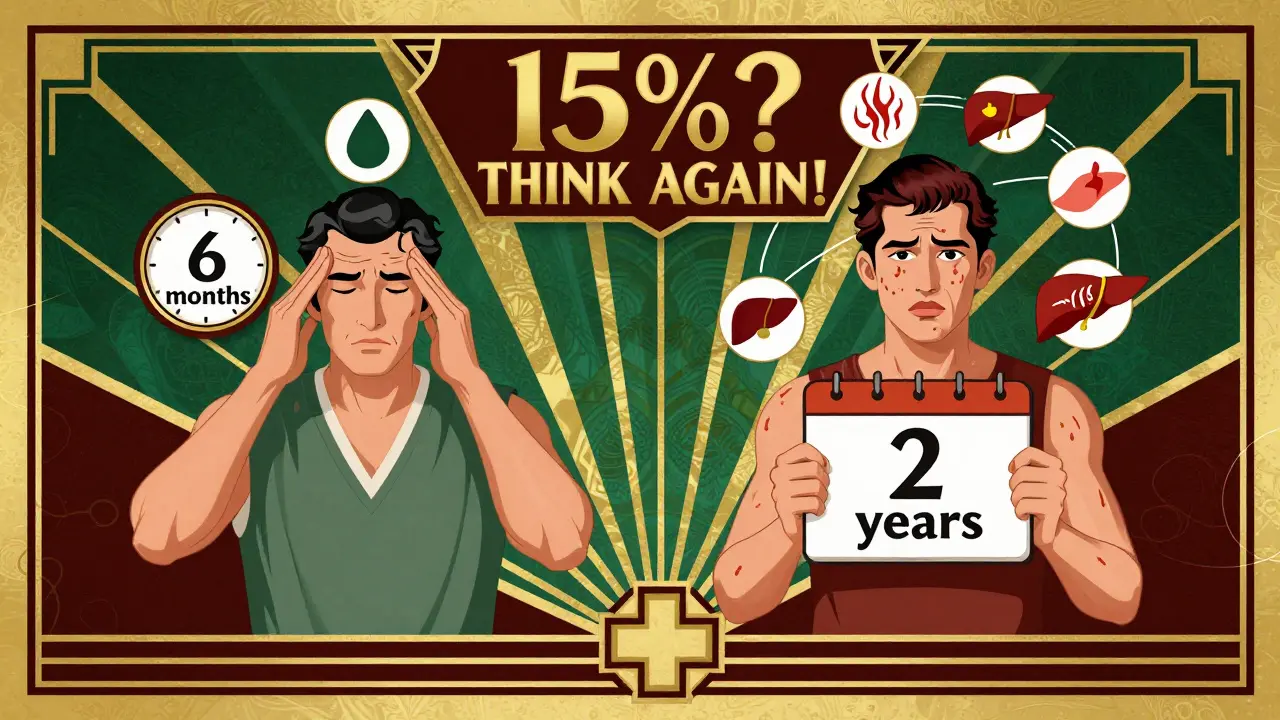
When you hear that a new drug caused headaches in 15% of patients, it sounds simple. But that number can be misleading. What if one group took the drug for 3 months and another took it for 2 years? The 15% might look the same, but the real risk? Totally different. This is why the FDA and top pharmaceutical companies are moving away from basic percentages and toward more accurate ways to measure safety in clinical trials.
Why Simple Percentages Fail
The most common way to report adverse events is called the Incidence Rate (IR). You take the number of people who had an adverse event, divide it by the total number of people in the study, and multiply by 100. Easy. But here’s the problem: IR ignores how long each person was actually exposed to the drug.Imagine two groups in a trial. Group A gets the drug for 6 months. Group B gets it for 24 months. In Group A, 10 people report nausea. In Group B, 30 people do. The IR is 20% for both if each group has 50 people. But that’s not fair. Group B had four times the exposure time. They were on the drug longer. More chances for side effects to show up. IR hides that. It makes the drug look equally risky, even though one group had far more time to react.
A 2010 analysis by Andrade showed IR underestimates true event rates by 18% to 37% in trials where treatment lengths vary. That’s not a small error. It’s enough to mislead doctors, regulators, and patients. The FDA noticed. In 2023, they requested exposure-adjusted data in a supplemental biologics license application - a clear signal that old methods are no longer enough.
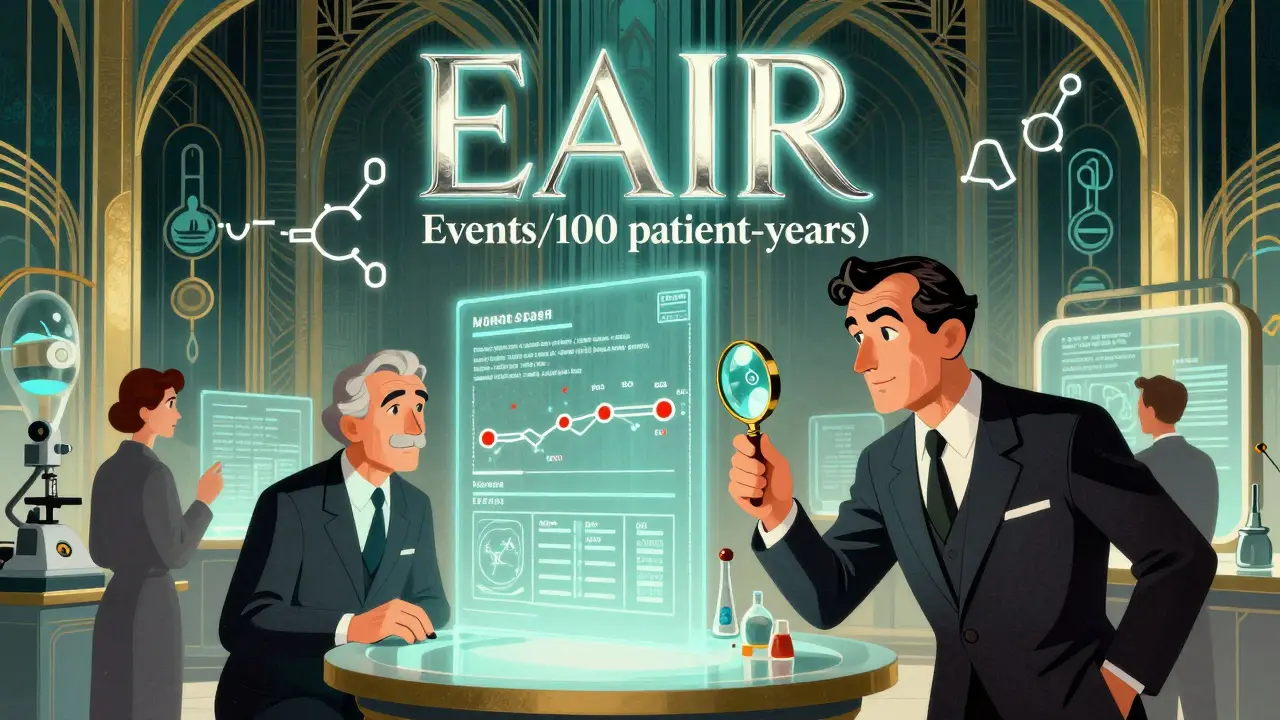
What Is Exposure-Adjusted Incidence Rate (EAIR)?
EAIR fixes the flaw. Instead of just counting people, it counts time. It asks: How many adverse events happened per 100 patient-years of exposure?Let’s break it down. A patient-year means one person taking the drug for one full year. If 10 people take the drug for 6 months each, that’s 5 patient-years (10 × 0.5). If one person takes it for 3 years, that’s 3 patient-years. You add them all up. Then you divide the total number of adverse events by that total time.
EAIR doesn’t just count events - it accounts for recurrence and variable exposure. If someone gets nausea twice in 18 months, EAIR counts both events. If someone drops out after 2 weeks, their time is only counted up to that point. This gives a real picture of risk over time.
MSD’s safety team found that switching to EAIR uncovered safety signals in 12% of their chronic therapy programs - signals that IR had completely missed. That’s huge. It means drugs that looked safe on paper might have hidden risks that only show up with longer exposure.
How EAIR Compares to Other Methods
There are three main ways to measure adverse events:- Incidence Rate (IR): Simple percentage. Total affected divided by total exposed. Ignores time.
- Event Incidence Rate (EIR): Events per 100 patient-years. Better than IR, but counts each event separately. If one person has 5 headaches, that’s 5 events - which can inflate the risk.
- Exposure-Adjusted Incidence Rate (EAIR): Events per 100 patient-years, with careful handling of exposure windows, treatment interruptions, and recurrence. Most accurate for complex trials.
EAIR is not perfect. It’s harder to calculate. A 2024 PhUSE survey found it takes 3.2 times longer to program EAIR in SAS than IR. And 35% of medical reviewers at Roche initially misunderstood it because they’d never seen it before.
But here’s the key: EAIR answers the right question. If you want to know how likely someone is to have a side effect per year of treatment, EAIR is the only method that gives you that. IR tells you how many people got sick. EAIR tells you how often sickness happens while on the drug.

Regulatory Shifts and Real-World Impact
The FDA’s 2023 request for EAIR wasn’t random. It followed years of warnings from experts. Dr. Gary Koch from UNC told the FDA Advisory Committee in 2022: "Failure to account for exposure time in adverse event reporting constitutes a fundamental statistical error that misrepresents drug safety profiles."ICH E9(R1), the global standard for clinical trial design, has required consideration of exposure time since 2020. But now, regulators are enforcing it. CDISC’s Oncology Therapeutic Area Guide (v3.0, 2023) now requires both IR and EAIR for serious adverse events. The FDA’s Biostatistics Review Template now includes checklists for exposure-adjusted methods - you have to document how you calculated time, and why you chose your method.
Industry adoption is accelerating. In 2020, only 12% of FDA submissions included exposure-adjusted metrics. By 2023, that jumped to 47%. The global clinical trial safety software market hit $1.84 billion in 2023, growing 22.7% year-over-year - mostly because companies are forced to upgrade their tools.
PhUSE, a global group of clinical programmers, released open-source SAS macros for EAIR in March 2023. They’ve been downloaded over 1,800 times. Users report an 83% drop in programming errors. That’s not just convenience - it’s reliability.
When EAIR Isn’t Enough: Competing Risks
There’s another layer. Sometimes, the reason a patient stops being monitored isn’t because they dropped out - it’s because they died. If you’re studying a drug for heart failure, and 20% of patients die during the trial, those deaths prevent you from seeing whether they’d have had kidney damage next. This is called a "competing risk."Traditional methods like Kaplan-Meier estimators don’t handle this well. They treat death as a "censored" event - meaning they pretend the patient just disappeared. But death isn’t missing data. It’s a competing outcome.
A 2025 study in Frontiers in Applied Mathematics and Statistics showed that using cumulative hazard ratio estimation instead of standard methods improved accuracy by 22% when competing events like death made up more than 15% of the data. This isn’t theory. It’s happening in trials for cancer, autoimmune diseases, and neurodegenerative conditions.
EAIR can still be used here - but it needs to be paired with cause-specific hazard models. The FDA’s Sentinel Initiative is already testing machine learning tools that combine EAIR with AI to detect safety signals earlier. Early pilots show 38% better detection than old-school methods.
What You Need to Know
You don’t need to run SAS code or calculate patient-years yourself. But if you’re reading a clinical trial report, knowing the difference matters.If a study only gives you IR, ask: "What was the average treatment duration?" If it’s less than 6 months, IR might be okay. If it’s over a year - especially if groups had different durations - demand EAIR. Look for phrases like "per 100 patient-years" or "exposure-adjusted." If you don’t see it, the safety data might be incomplete.
Pharmaceutical companies are now required to justify their choice of method. The EMA accepts IR or EAIR, but only if you explain why. The FDA is moving toward EAIR as the gold standard. And by 2027, experts predict 92% of Phase 3 submissions will include it.
This isn’t just about statistics. It’s about trust. When a drug is approved, people’s lives are on the line. A misleading number isn’t a technical glitch - it’s a risk to public health. Better methods mean better decisions. And that’s what the FDA, the industry, and patients all want.
What’s Next?
The FDA’s 2024 draft guidance on exposure-adjusted analysis is open for public comment. PhUSE is finalizing an R-based reference implementation for EAIR, due in early 2025. Training demand is up 148% since 2021. This isn’t a trend. It’s a transformation.Don’t just look at the percentage. Look at the time. Because safety isn’t about how many people got sick. It’s about how often they got sick - while they were taking the drug.
What’s the difference between incidence rate and exposure-adjusted incidence rate?
Incidence Rate (IR) is a simple percentage: number of people who had an adverse event divided by total people in the study. It doesn’t consider how long each person was exposed. Exposure-Adjusted Incidence Rate (EAIR) calculates events per 100 patient-years - meaning it accounts for how long each person took the drug. EAIR gives a more accurate picture of risk over time, especially when treatment durations vary between groups.
Why does the FDA prefer EAIR now?
The FDA prefers EAIR because traditional methods like IR can hide real safety risks. In trials where some patients stay on a drug for years and others drop out early, IR makes the drug look safer than it is. EAIR corrects this by factoring in actual exposure time. In 2023, the FDA requested EAIR in a regulatory submission - a clear signal that they now expect this level of detail for accurate safety assessment.
Can EAIR be used for all types of adverse events?
EAIR works best for events that can happen multiple times or over long periods, like nausea, rash, or elevated liver enzymes. For rare, one-time events like anaphylaxis, IR may still be useful. But when exposure time varies significantly - especially in chronic disease trials - EAIR is the preferred method. It’s also critical when competing risks like death are involved, though it must be combined with hazard modeling in those cases.
Is EAIR harder to calculate than traditional methods?
Yes. EAIR requires detailed tracking of each patient’s start and end dates of treatment, including interruptions. Programming it in tools like SAS or R takes about 3 times longer than calculating IR. Common errors include incorrect date handling, ignoring treatment breaks, or miscounting patient-years. Many companies now use standardized, open-source macros to reduce mistakes.
Should I trust a clinical trial that only reports IR?
Be cautious. If the trial lasted less than 6 months and all participants were exposed for roughly the same time, IR might be acceptable. But if treatment durations varied - or if the drug is meant for long-term use - IR alone is insufficient. Regulatory agencies are moving toward EAIR, and transparency about exposure time is now expected. If a study doesn’t provide it, the safety data may be incomplete or misleading.
James Dwyer
January 28, 2026 AT 04:57This is exactly why I stopped trusting pharma press releases. They love to bury the real risk under pretty percentages. I’ve seen this in my own family’s meds - the ‘10% chance of side effects’ turned into someone on the drug for 18 months getting hit twice. That’s not 10%. That’s a pattern.
EAIR isn’t just fancy stats - it’s honesty. If you’re going to prescribe something for years, we deserve to know how often it actually breaks down over time, not just who got sick first.
jonathan soba
January 28, 2026 AT 07:04Let’s be real - IR is lazy. It’s the statistical equivalent of saying ‘50% of people who ate sushi got sick’ without mentioning whether they ate it once or every day for a year. The FDA’s shift to EAIR is long overdue, but don’t expect industry to embrace it willingly. It exposes too many drugs that look safe on paper but are slow-burn disasters.
And yes, it takes longer to calculate. Good. If it’s hard, that’s the point. Safety shouldn’t be a quick Excel formula.
Kathy Scaman
January 29, 2026 AT 19:19I work in clinical ops and can confirm - EAIR changed everything for us. We had this one drug that looked perfect in Phase 2 with a 5% headache rate. But when we ran EAIR, we realized the headaches spiked after 9 months. We almost missed it. Now we flag any trial over 6 months for exposure-adjusted analysis. It’s not glamorous, but it saves lives.
Also, the open-source SAS macros from PhUSE? Life saver. My team used to waste weeks debugging date logic. Now it’s automated. Thank you, PhUSE.
Anna Lou Chen
January 31, 2026 AT 02:10Ah, the neoliberal epistemological collapse of pharmacovigilance. The IR paradigm is a symptom of late-stage biomedical capitalism - commodifying risk as a discrete, decontextualized metric, reducing human temporality to a flat binary: sick or not sick.
EAIR, by contrast, reintroduces phenomenological duration into the equation. It acknowledges that the body is not a static container but a dynamic, temporally embedded organism. The patient-year is not just a unit - it’s a hermeneutic of lived exposure.
And yet, even EAIR fails to account for the ontological weight of iatrogenesis. We still treat adverse events as ‘events’ - as if nausea were an external intrusion rather than the body’s own epistemic resistance to chemical colonization.
Next up: the dialectical synthesis of EAIR with Heideggerian care-structures. I’m writing the paper.
Lance Long
January 31, 2026 AT 17:27Hey, if you’re reading this and you’re a patient or a caregiver - this matters. A lot.
That ‘15% chance of headaches’? If you’re on the drug for 3 years, that’s not 15%. That’s maybe 40-60% cumulative risk. EAIR tells you that. IR hides it.
Don’t let your doctor skip this. Ask: ‘What’s the patient-year rate?’ If they look confused, they’re probably using old-school numbers. Push for the real data. Your body deserves better than a statistic that ignores time.
Timothy Davis
January 31, 2026 AT 19:50EAIR is still garbage. You’re counting events per patient-year, but what if someone has 12 nausea episodes in 6 months? EAIR treats them as 2 events per year - but that’s not the same as someone who has 2 episodes over 2 years. EIR is better. And even EIR ignores clustering.
And don’t get me started on how they handle missing data. Half the time, the ‘exposure time’ is estimated from electronic records that don’t even track when the patient stopped taking the pill. You’re building a house on sand.
What we need is a Bayesian hierarchical model with time-varying covariates. But nope - we get EAIR because it sounds fancy and the FDA said so.
fiona vaz
February 1, 2026 AT 11:03For anyone wondering if this is worth the extra work - yes. I’ve reviewed dozens of trial packages. The ones that include EAIR are always more trustworthy. Not because they’re perfect, but because they show they care enough to do the hard thing.
And if you’re a researcher - please, just use the PhUSE macros. Don’t reinvent the wheel. We’ve all made the same date-handling mistakes. Save your sanity.
Sue Latham
February 2, 2026 AT 05:42Oh honey, you’re telling me the pharma companies didn’t just make up numbers to sell drugs? Shocking.
I knew it. I knew it. I’ve been saying this for years - if they told you the truth, you’d never take anything. ‘Oh, this pill gives you migraines 3x a week after 8 months? But hey, 80% of people didn’t get sick in the first 3 months!’
So now they’re making it harder to lie? Cute. I’ll believe it when I see a drug company voluntarily publish EAIR before they’re forced to.
Mark Alan
February 2, 2026 AT 21:39AMERICA IS THE ONLY COUNTRY THAT GIVES A DAMN ABOUT REAL SAFETY DATA 😤🇺🇸
EUROPE? They still use IR like it’s 2005. CHINA? They don’t even report adverse events. But here? We’re leading the world in honest science. EAIR? That’s American innovation right there. Nobody else has the guts.
Stay woke. Stay safe. Stay USA. 🇺🇸🔥
Amber Daugs
February 4, 2026 AT 09:52So let me get this straight - you’re telling me that before, drug companies were lying to patients by hiding how often side effects actually happen over time? And now they’re being forced to tell the truth?
Wow. I’m just so proud of humanity right now. 🙃
But seriously - if your doctor still uses IR, they’re either lazy or complicit. Ask them. Right now. Don’t wait until you’re on the drug for a year and your liver is screaming.
Ambrose Curtis
February 6, 2026 AT 03:30EAIR is the real deal. I used to work in biostats and we used to laugh at IR - it was like measuring how many people got wet in a rainstorm without saying how long they stood outside.
Yeah, it’s harder. Yeah, the software sucks. But we fixed it. PhUSE macros are gold. And if you’re a reviewer who doesn’t get it - go take the training. It’s free. Don’t be the person who approves a drug because someone typed ‘20%’ into Excel and called it a day.
Linda O'neil
February 6, 2026 AT 06:47This is why I love science when it gets real. No fluff. No spin. Just: ‘Here’s how often this actually breaks your body over time.’
If you’re a patient - demand EAIR. If you’re a doctor - push for it. If you’re in pharma - stop cutting corners. We’re not just crunching numbers. We’re deciding who lives and who doesn’t.
Robert Cardoso
February 8, 2026 AT 04:40EAIR is just a Band-Aid. The real problem is that we’re testing drugs on people who are too sick to begin with. If you’re studying a drug for terminal cancer, and 30% of patients die in 6 months - the ‘headache rate’ is meaningless. You’re not measuring drug toxicity. You’re measuring how fast the disease kills them.
Stop pretending EAIR solves everything. It just makes the lie look more sophisticated.
Katie Mccreary
February 8, 2026 AT 20:17SRI GUNTORO
February 10, 2026 AT 02:26Western medicine is broken. You measure sickness like a machine, not a soul. EAIR? It’s still a number. It doesn’t ask why the body reacts. It doesn’t heal. It just calculates. You think statistics fix pain? You think patient-years fix suffering?
True healing begins when we stop counting and start listening.