Weight Gain from Antidepressants: Which Drugs Cause It and How to Stop It
 Dec, 9 2025
Dec, 9 2025
Antidepressant Weight Gain Estimator
Estimate your potential weight gain based on antidepressant type and treatment duration. Data from Harvard Health (2024) study.
Enter your medication and duration to see estimated weight gain
It’s not uncommon to hear someone say, "I started taking antidepressants and suddenly I couldn’t stop eating." This isn’t just a personal complaint-it’s a well-documented effect. Around 55 to 65% of people on long-term antidepressant treatment gain weight, according to a 2023 review in PMC. For many, this isn’t just about clothes fitting tighter. It’s about increased risk for diabetes, heart disease, and even relapsing into depression because they stop taking their meds.
Why Do Antidepressants Make You Gain Weight?
It’s not one simple reason. Antidepressants change how your brain handles serotonin, dopamine, and other chemicals that control hunger, mood, and energy use. At first, some people actually lose weight because their appetite drops. But after six to twelve months, things flip. Serotonin receptors in your brain get less sensitive. Your body starts craving carbs-especially sugary, starchy foods like bread, pasta, and cookies. That’s not weakness. That’s biology. Some antidepressants also slow down your metabolism. They interfere with how your body uses glucose and insulin, making it harder to burn calories. Others, like mirtazapine and tricyclics, bind to histamine receptors, which directly triggers hunger. Even your stress hormones play a role. Depression and obesity both mess with the HPA axis-the system that controls cortisol. So when you’re on antidepressants and stressed, your body is primed to store fat.Which Antidepressants Are Most Likely to Cause Weight Gain?
Not all antidepressants are the same when it comes to weight. Some are nearly neutral. Others are practically guaranteed to add pounds over time.- High risk: Amitriptyline, nortriptyline, imipramine (tricyclics), mirtazapine (Remeron), paroxetine (Paxil), phenelzine (Nardil)
- Moderate risk: Citalopram (Celexa), escitalopram (Lexapro), sertraline (Zoloft), duloxetine (Cymbalta)
- Lowest risk / weight neutral or loss: Bupropion (Wellbutrin)
| Medication | Weight Gain at 6 Months | Weight Gain at 24 Months |
|---|---|---|
| Bupropion | 0.25 lb loss | 1.2 lb gain |
| Sertraline | 0.5 lb gain | 3.2 lb gain |
| Escitalopram | 1.4 lb gain | 3.6 lb gain |
| Paroxetine | 1.4 lb gain | 2.9 lb gain |
| Duloxetine | 1.2 lb gain | 1.7 lb gain |
Is It Really the Medication-or Just Feeling Better?
This is where things get tricky. Many people start antidepressants because they’ve lost their appetite due to depression. They’re not eating. They’re losing weight. When the meds start working, their mood lifts-and so does their appetite. That’s not the drug causing weight gain. That’s their body returning to normal. A study from the Mayo Clinic points this out clearly: some of the weight gain you see isn’t from the pill. It’s from your brain finally letting you eat again. So before you blame the medication, ask: "Was I eating enough before?" If you were underweight or barely eating, some of the gain is recovery-not side effect. But if you were eating normally before and now you’re constantly hungry, craving snacks, or gaining weight even though your appetite hasn’t changed, then the drug is likely the main driver.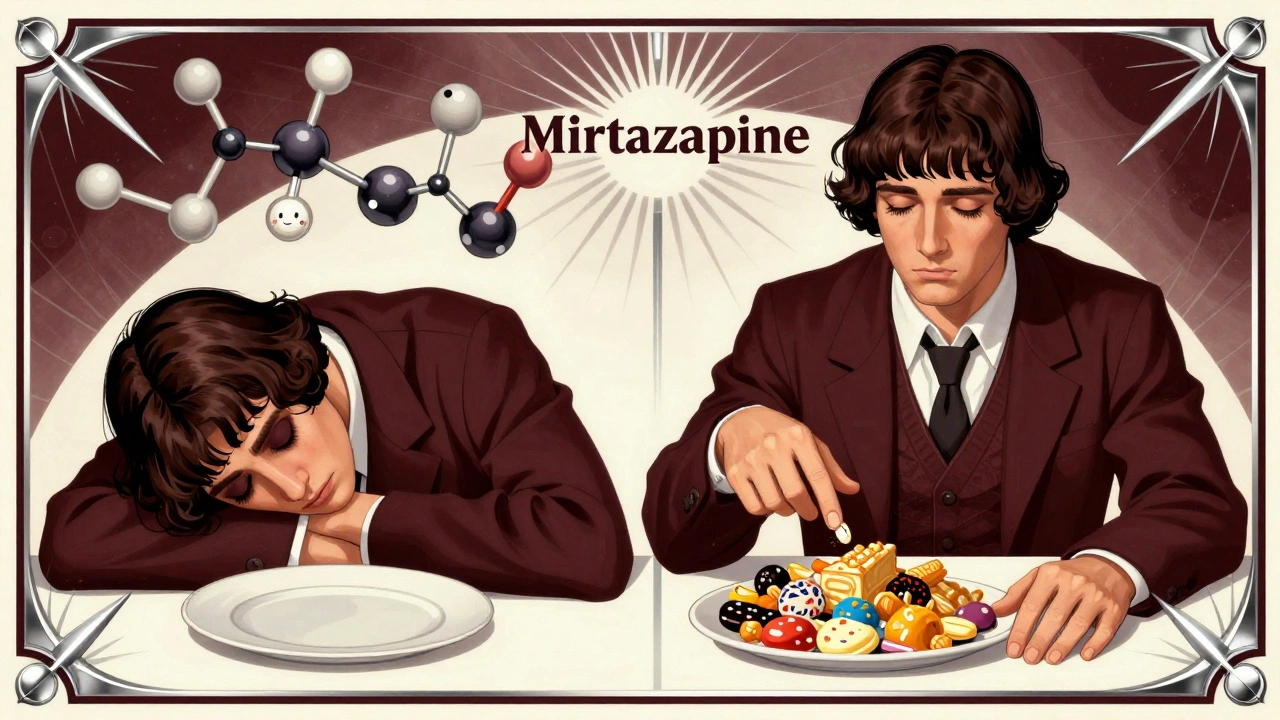
What Can You Do About It?
Never stop your antidepressant because of weight gain. Stopping suddenly can trigger severe withdrawal, anxiety, or even a return of depression. In fact, studies show that people who quit because of weight gain are 30-50% more likely to relapse. Instead, talk to your doctor. Here are four proven strategies:- Switch to a weight-neutral option - If you’re on paroxetine or mirtazapine and gaining weight, ask about switching to bupropion. It’s not right for everyone (it can raise blood pressure or cause insomnia), but for many, it’s the best alternative.
- Add metformin - This diabetes drug helps your body use insulin better. Studies show it cuts antidepressant-related weight gain by up to 50%. It’s safe, cheap, and often covered by insurance.
- Try GLP-1 agonists - Drugs like semaglutide (Wegovy) and liraglutide (Saxenda), originally for diabetes and obesity, are now being used off-label for this exact problem. Clinical trials show patients on antidepressants lost 5-7% of their body weight when added to these drugs.
- Change your habits - No pill fixes a poor diet. Focus on protein, fiber, and complex carbs. Avoid sugary drinks and processed snacks. Even small changes-like walking 30 minutes a day-can offset metabolic slowdown.
Genetics and Your Risk
Not everyone gains weight on the same drug. Why? Genetics. Some people have a variation in the CYP2C19 gene that affects how quickly their body breaks down certain antidepressants. Slow metabolizers end up with higher drug levels in their blood-meaning more side effects, including weight gain. If you’ve gained weight on multiple antidepressants, ask your doctor about genetic testing. It’s not routine yet, but it’s becoming more common in mental health clinics. Knowing your metabolism type can help pick the right drug from the start.What About Long-Term Effects?
Here’s something alarming: research published in Nature suggests that antidepressants might leave a lasting mark on your metabolism-even after you stop taking them. In animal studies, stress combined with antidepressant use, followed by a high-fat diet, led to extreme weight gain long after the drugs were gone. This doesn’t mean you’ll automatically become obese. But it does mean that if you’ve been on antidepressants for over a year, your body might be more sensitive to weight gain from poor diet or inactivity-even years later. That’s why managing your lifestyle doesn’t end when you stop the medication.Bottom Line: You Have Options
Weight gain from antidepressants isn’t inevitable. It’s not your fault. And it’s not something you have to live with. If you’re on a high-risk drug like paroxetine or mirtazapine and gaining weight, talk to your doctor about switching. If you’re on sertraline or escitalopram and seeing slow gains, consider adding metformin. If you’re still unsure, bupropion is your safest bet for avoiding weight gain. And remember: your mental health matters more than the number on the scale. But you don’t have to choose between feeling better and staying healthy. With the right approach, you can do both.Do all antidepressants cause weight gain?
No. While many antidepressants can lead to weight gain over time, bupropion (Wellbutrin) is the only commonly prescribed one that consistently leads to weight loss or neutrality in the first six months. Even after two years, it causes significantly less weight gain than drugs like paroxetine or mirtazapine.
How soon after starting antidepressants do you start gaining weight?
Weight gain usually doesn’t happen right away. Most people see little to no change in the first 1-3 months. The real shift happens after six months, when serotonin receptors in the brain become less responsive. By 12-24 months, most people on high-risk drugs have gained noticeable weight.
Can I lose the weight I gained from antidepressants?
Yes, but it often requires more than diet and exercise alone. Many people find that adding metformin or a GLP-1 agonist helps reverse the metabolic changes caused by the medication. Lifestyle changes are essential, but they work better when paired with targeted medical support.
Should I stop my antidepressant if I’m gaining weight?
No. Stopping abruptly can trigger withdrawal symptoms and increase your risk of depression returning by 30-50%. Instead, talk to your doctor about switching medications, adding a weight-management drug, or adjusting your lifestyle. You don’t have to choose between mental health and physical health.
Is bupropion safe for everyone?
Bupropion is generally safe but not ideal for everyone. It can raise blood pressure, cause insomnia, or trigger anxiety in some people. It’s also not recommended for those with a history of seizures or eating disorders. Your doctor will assess your medical history before prescribing it.
Does therapy help with weight gain from antidepressants?
Yes. Cognitive behavioral therapy (CBT) can help rewire your relationship with food, reduce emotional eating, and build sustainable habits. When combined with medication changes or metformin, therapy significantly improves long-term weight outcomes.
Are there any natural remedies that help?
There’s no proven natural supplement that directly counteracts antidepressant-induced weight gain. However, regular physical activity, high-protein diets, and adequate sleep can support metabolism. Avoid unregulated supplements marketed for weight loss-they can interact dangerously with antidepressants.
How common is weight gain from antidepressants?
It’s very common. Studies show 55-65% of people on long-term antidepressant treatment gain weight. For some, it’s just a few pounds. For others, it’s 10, 20, or more pounds over several years. It’s one of the top reasons people stop taking their medication.
Iris Carmen
December 11, 2025 AT 06:32lol i started zoloft and suddenly i was eating entire pizzas at 2am like it was normal. not even hungry, just... compulsive. my jeans cried.
Shubham Mathur
December 12, 2025 AT 15:42you people act like weight gain is the end of the world but if you were depressed and not eating for months then suddenly you can enjoy food again thats not a side effect thats recovery
also bupropion is great but if you have anxiety itll make you feel like your brain is on fire
Nikhil Pattni
December 14, 2025 AT 11:57yo i was on mirtazapine for 18 months and gained 47 lbs and honestly i dont even care anymore i just eat everything now like a bear prepping for hibernation 🐻❄️
also i tried metformin and it made me feel like i swallowed a whole bag of sour candy so i stopped but my doc says its still the best bet if you can handle the stomach drama
and dont even get me started on those GLP-1 drugs like we're all just gonna start injecting ourselves with weight loss potions like its a trend on tiktok
also genetics? yeah my mom gained weight on every antidepressant she ever took so its definitely in the bloodline
and bupropion? i tried it and it gave me insomnia so bad i started talking to my cat at 3am like we were in a therapy session
Noah Raines
December 16, 2025 AT 05:51same. i was on lexapro for a year and gained 15 lbs. i thought i was just lazy but turns out my brain was basically begging for donuts.
switched to wellbutrin and lost 8 lbs in 3 months. no magic, just no more 3am cookie raids 🙌
Stacy Tolbert
December 17, 2025 AT 05:08i hate that this is so common but no one talks about how it makes you feel like a failure even when you know it’s not your fault
i cried in the grocery store last week because i couldn’t decide between oat milk and almond milk and then i bought three bags of gummy bears just to feel something
it’s not just the weight. it’s the shame. the constant whispering in your head that you’re not trying hard enough
and then you take a shower and your skin looks different and you feel like a stranger in your own body
i wish doctors would warn you about this before they hand you the script
Maria Elisha
December 17, 2025 AT 19:41why is this even a thing? just stop taking them.
Larry Lieberman
December 19, 2025 AT 05:13my therapist said my weight gain was "emotional eating" but honestly i just crave carbs now like my brain rewired itself to need them
and yes i know bupropion is the "good one" but i tried it and it made me feel like a robot on espresso ☕️🤖
Morgan Tait
December 19, 2025 AT 11:12you know what they’re not telling you? Big Pharma knows antidepressants cause weight gain so they push the metformin and GLP-1 drugs too - it’s a two-punch profit model
they sell you the pill that makes you gain weight… then sell you the pill to fix it
and don’t get me started on how the FDA lets this slide while banning herbal supplements that might actually help
it’s not a medical issue - it’s a corporate one
they don’t care if you’re diabetic - they care if your insurance pays for the next script
and don’t even think about asking for bupropion unless you’re white and middle class - try asking as a black man and see how fast your doctor says "it might trigger anxiety"
Chris Marel
December 20, 2025 AT 12:32i’m from nigeria and here, antidepressants are still kinda stigmatized
but when my cousin started on sertraline, she gained weight and her family blamed her for "not praying enough"
she didn’t tell anyone it was the meds - she just stopped taking them and went back into a dark place
we need more education - not shame
and thank you for mentioning metformin - i didn’t know it could help with this
Brianna Black
December 22, 2025 AT 03:20As someone who has spent two decades in clinical psychology and has published peer-reviewed work on neuroendocrine pathways in mood disorders, I must emphasize that the reductionist framing of this issue as merely "medication-induced weight gain" is both scientifically inadequate and ethically irresponsible.
The conflation of metabolic dysregulation with behavioral causality - particularly in the absence of longitudinal biomarker data - perpetuates a dangerous myth that patients are passive recipients of pharmacological fate.
The HPA axis, serotonin receptor downregulation, and insulin sensitivity are not linear phenomena. They are dynamic, bidirectional systems influenced by circadian rhythm, dietary micronutrient density, gut microbiota composition, and psychosocial stressors that are rarely, if ever, controlled for in population studies.
Moreover, the assertion that bupropion is "weight neutral" is misleading. In patients with comorbid ADHD or nicotine dependence, it frequently induces anorexia and muscle catabolism - a form of metabolic harm equally concerning.
And while GLP-1 agonists show promise, their long-term neurocognitive effects on serotoninergic pathways remain entirely unexplored.
To suggest that patients should "switch" or "add" without considering individual phenotypes is not medical advice - it is pharmaceutical arbitrage disguised as empowerment.
The real solution lies not in pharmacological gymnastics, but in integrated care models that prioritize nutritional psychiatry, trauma-informed movement, and epigenetic literacy - none of which are reimbursable under current insurance frameworks.
And yes, I am aware that this comment will be downvoted into oblivion.
Andrea Beilstein
December 22, 2025 AT 22:13we treat depression like a broken lightbulb you just swap out for a new one
but the soul doesn’t work that way
maybe the weight gain isn’t the side effect
maybe it’s the body screaming that the medication isn’t fixing the root
maybe we’re not supposed to be numb
maybe we’re supposed to feel hungry - for connection, for meaning, for food that nourishes not just the body but the silence inside
and maybe the real question isn’t which drug causes weight gain
but why we’re so afraid to sit with the hunger
precious amzy
December 23, 2025 AT 11:05Ah, yes - the classic neoliberal solution: swap one pharmaceutical dependency for another, then add a wellness influencer’s protein shake on top. How very… efficient.
Metformin? GLP-1 agonists? Please. You’re not treating depression. You’re treating the symptom of a culture that pathologizes embodiment and commodifies healing.
The fact that we’ve reduced existential suffering to a metabolic equation - and then monetized the fix - is not a triumph of medicine.
It’s a funeral.